Ventricular Septal Defect (VSD)
VSD is an opening of the ventricular septum causing communication between the two ventricles. Most (80% of cases) are perimembranous defects.
Incidence: VSD is the most common cardiac defect, accounting for nearly one-third of all heart defects.
Sonographic findings:
Fig 1, Fig 2
- Perimembranous and subaortic VSD are best visualized with a left outflow tract view and best imaged when the ultrasound beam is perpendicular to the focused septum.
- Muscular defects, which are difficult to observe, are best searched for in the short-axis view by trying to demonstrate a connection between the two ventricles.
- Color Doppler is helpful in demonstrating shunting across the septum.
- Color Doppler spatiotemporal image correlation has the potential to simplify visualization of the location and extent of ventricular septal defects.
- Pitfalls:
- Defects smaller than 1-2 mm will escape detection.
- False dropout is most likely to occur when the ultrasound beam is parallel to the defects.
- Isolated VSD is one of the common defects rarely diagnosed correctly, especially on routine screening at 18 weeks.
- Usually diagnosable between 16 and 18 weeks, but diagnosis possible at 14 weeks with transvaginal ultrasound.
- Some cases may show thickened NT between 11 and 14 weeks.
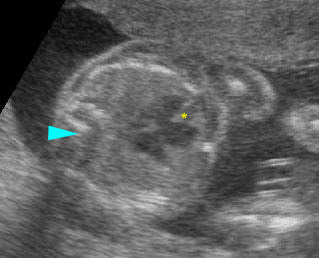
Large ventricular septal defect: Four-chamber view: incomplete interventricular septum (*), (arrowhead = spine)
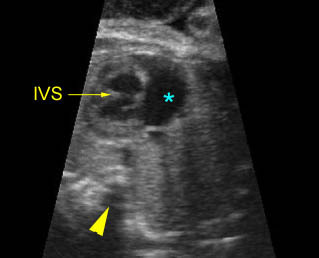
ASD & VSD: Atrial septal and ventricular septal defect
Four-chamber view: abnormal cardiac axis, no atrial septum (*) and incomplete ventricular septum (arrowhead = spine)
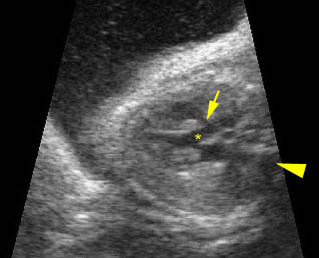
Ventricular septal defect: Long axis view: small interventricular defect (arrow) (not seen in the four-chamber view) (* = aortic root, arrowhead = spine)
Associations: May occur alone or be associated with certain syndromes or other heart abnormalities including tetralogy of Fallot and transposition of the great vessels. VSD is also associated with increased risk of aneuploidy, even seemingly isolated VSD.
Management: Careful prenatal and postnatal search for associated anomalies is required. All continuing pregnancies should be karyotyped. Isolated VSD should not alter standard obstetric care.
Prognosis: Usually good for isolated and mild forms, but poor when associated with associated defects and large defects, especially the prenatally diagnosed defects. Ventricular septal defect can undergo spontaneous closure in utero, especially defects of <3 mm.
Recurrence risk: Most are multifactorial with a recurrent risk of 2-4%.

