Pulmonary Hypoplasia
Pulmonary hypoplasia is a disorder characterized by a decrease in the number of lung cells, airways, and alveoli, resulting in a decrease in lung size and weight as well as in the lung weight to body weight ratio. Of all the clinical situations in which pulmonary hypoplasia is a concern, the most common is oligohydramnios resulting from preterm premature rupture of membranes (PPROM) and renal agenesis. However, pulmonary hypoplasia can result from a pressure effect or pleural effusion from any causes or masses in the thorax. The reduction in breathing movements may also contribute to the development of pulmonary hypoplasia.
Incidence: 1.4 per 1000 births.
Sonographic findings:
Fig 1, Fig 2
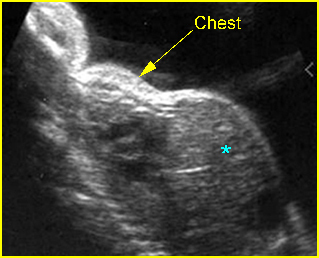
Fig 1: Lung hypoplasia Sagittal scan of the trunk: small thorax compared with abdomen (*) in association with chondroectodermal dysplasia
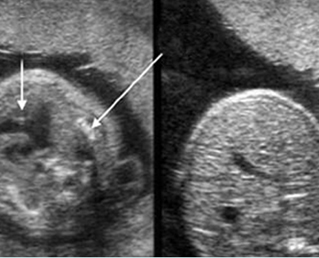
Fig 2: Lung hypoplasia Cross-sectional scan of the thorax and abdomen: small thorax with atrial septal defect (short arrow) and severely short rib (long arrow) in association with Jeune syndrome, compared to abdomen (right)
Video clips of lung hypoplasia
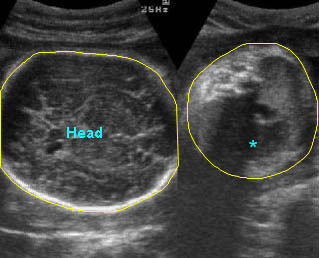
Lung hypoplasia / SRP Syndrome: Small thorax (*) with short ribs compared to the head size in case of fetal short-rib polydactyly syndrome
- Small thorax: thoracic circumference (TC) measurements are obtained in the transverse plane at the level of the four-chamber view of the heart. The ratio of TC to abdominal circumference (AC), HC or TC/femur length (FL) is useful in the diagnosis of pulmonary hypoplasia. These ratios are fairly constant, especially the TC/AC ratio which appears to have the least variability and has been shown to be >0.80 in nearly all normal fetuses after midpregnancy. This serial ratio measurement is a reliable predictor of pulmonary hypoplasia. However, the accuracy for prediction is relatively low if the hypoplasia is secondary to preterm rupture of membranes or a pressure effect from mass or pleural effusion.
- The ratio of chest length, defined from the top of the thorax to the top of the diaphragm, to trunk length, defined from the top of the thorax to the bottom of the urinary bladder, is highly predictive for postnatal respiratory conditions related to pulmonary hypoplasia.
- Lung size: direct measurement of the lung appears to be more sensitive than the TC/AC ratio, and is useful in the case of pressure effects such as diaphragmatic hernia. The lung area (thoracic area-cardiac area/100) had sensitivity and specificity of 85%. With 3D ultrasound, fetal lung volume measurements can be undertaken interchangeably using the multiplanar technique or the rotational method with VOCAL. However, this technique is still preliminary.
- Doppler studies of the main stems of the pulmonary arteries may be useful. Increased pulsatility index (PI) or an abnormal acceleration time/ejection time ratio are useful in predicting lung hypoplasia, especially when combined with clinical and biometric parameters. A preliminary study showed that fetal pulmonary vascular reactivity testing with maternal hyperoxygenation is highly predictive of pulmonary hypoplasia. A reactive test predicted that 92% of infants would survive; a non-reactive test predicted 79% fetal deaths from pulmonary hypoplasia.
- Fetal breathing movements may be used as a predictor of favorable neonatal outcome, and as an adjunct in the diagnosis of pulmonary hypoplasia. However, several factors affect fetal breathing, including the time of day, smoking, drugs and glucose load.
- Oligohydramnios in most cases (related to PPROM): the amniotic fluid index is an important independent predictor of neonatal pulmonary hypoplasia.
- Occasionally, associated causes of the pressure effect such as pleural effusion, and masses from various causes.
- Occasionally, skeletal dysplasias such as osteogenesis imperfecta type II, short-rib polydactyly syndrome, Jeune syndrome, etc.
- MR images may be a promising method for predicting fetal pulmonary hypoplasia.
Associations: Prolonged oligohydramnios, chest masses, pleural effusion, and skeletal dysplasia.
Prognosis: Relatively poor overall and depending on associated abnormalities.

