Tetralogy of Fallot (TOF)
TOF consists of four anatomical malformations as follows: (1) ventricular septal defect; (2) pulmonary artery stenosis; (3) aortic valve that overrides the interventricular septum; and (4) hypertrophy of the right ventricle, which may not occur until the newborn period.
Fig 1
Incidence: 0.2-0.3 in 1000 live births, accounting for 7% of structural cardiac defects.
Sonographic findings:
Fig 2, Fig 3, Fig 3, Fig5
- Very large aortic root (the most common prenatal sonographic finding).
- Normal aortic root excluding TOF.
- Small pulmonary artery or stenosis of the right ventricular outflow tract.
- Ventricular septal defect in the outlet portion of the septum and an overriding aorta, best seen in long-axis views.
- Right ventricular hypertrophy.
- Hydrops fetalis or polyhydramnios may be seen in the absence of the pulmonary valve.
- Increased NT especially in fetuses with chromosomal 22q11 deletion.
- Although Doppler studies show increased peak velocities in the pulmonary artery, suggestive of obstruction of blood flow in the right outflow tract, normal pulmonic velocity in TOF is commonly observed due to the parallel flow circulations created by the combination of ventricular septal defect and ductus arteriosus.
- Reversal of flow in the arterial duct and failure of growth of the pulmonary trunk predict the need for early surgery to maintain pulmonary blood flow.
- Pitfalls:
- A frequent artifact resembles overriding of the aorta.
- Overiding of the aorta can also be seen in double-outlet right ventricle, truncus arteriosus, or transposition of great arteries.
- Usually diagnosed after 16-18 weeks, but possible after 13-15 weeks with transvaginal ultrasound in some cases.
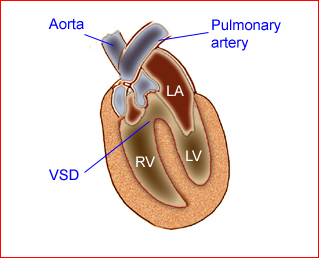
Fig 1: Schematic drawing of Tetralogy of Fallot (LA = left atrium, LV = left ventricle, RV = right ventricle, VSD = ventricular septal defect)
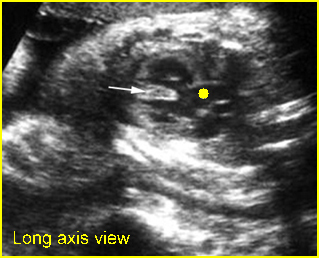
Fig 2: Overriding aorta (in case of TOF) Long axis view of the heart: aortic root (solid circle) running from both ventricles (arrow = interventricular septum)
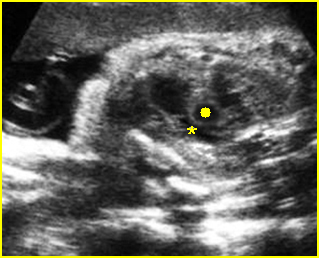
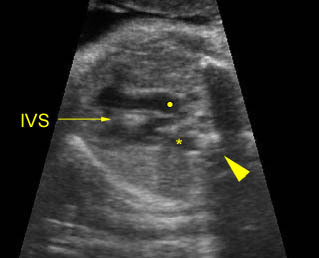
Fig 3: Pulmonary stenosis (in case of TOF) Long axis view of the heart: small pulmonary trunk (*) compared to aortic root (solid circle)
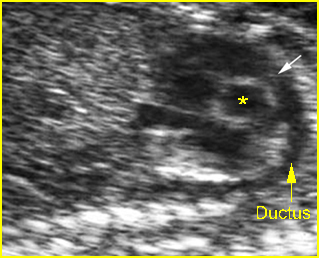
Fig 4: Small Pulmonary trunk and ductal arch Short axis view: Small ductal arch (arrow) giving no branch to the head (* = ascending aorta)
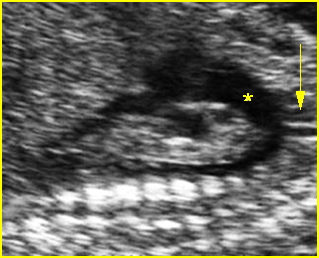
Fig 5: Large aortic arch Large aorta compared to ductal arch: aortic arch (*), giving the carotid branch (arrow) to the head
Video clips of Tetralogy of Fallot (TOF)
Overding aorta: Longitudinal scan of the aoratic arch; * overiding aorta, solid circle = aortic arch, arrow = right ventricle
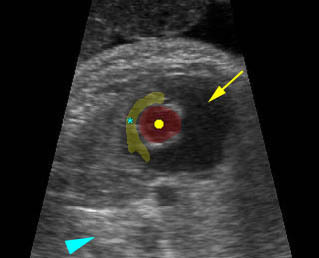
Pulmonary stenosis: Short-axis view: very small pulmonary artery (*) compared to ascending aorta (solid circle), arrow = right ventricle, arrowhead = spine
Associations: Other abnormalities, and chromosomal abnormalities found in 60% of cases. Chromosome 22q11 microdeletion may be seen in 11-34% of cases.
Management: Careful prenatal and postnatal search for associated anomalies and karyotype (including FISH for chromosome 22q11 deletion) are indicated. Delivery should be performed where immediate pediatric cardiac consultation is available.
Prognosis: Good prognosis in the case of a normal pulmonary valve, with surgical correction; poor prognosis if the pulmonary valve is absent which is related to hydrops fetalis.

