Diaphragmatic Hernia
Diaphragmatic hernia (CDH) is a herniation of abdominal viscera into the fetal chest, which results from a congenital defect in the fetal diaphragm. The most common location is posterolateral (Bockdalek) on the left side (85-90%) followed by a retrosternal (foremen of Morgagni hernia) defect.
Incidence: 1 in 2500-4000 chromosomally normal fetuses.
Fig 1, Fig 2, Fig 3
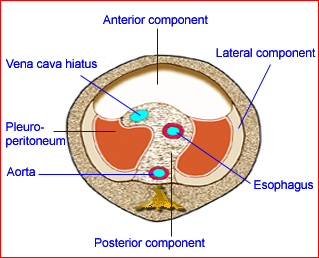
Fig 1: Schematic drawing: Developmental components of the diaphragm
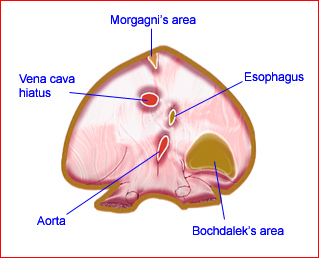
Fig 2: Schematic drawing of the diaphragm seen from below; note the location of potential site of Bochdalek’s hernia
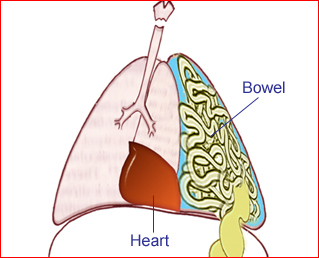
Fig 3: Schematic drawing: Diaphragmatic hernia: bowel loops in the chest with mediastinal shift
Sonographic findings:
Fig 3, Fig 4, Fig 5, Fig 6
- Abdominal organs above diaphragm, visualization of peristalsis.
- Mediastinal shift, heart displacement to the right side.
- 90% of left CDH detected due to visualization of displaced heart and stomach in the chest.
- Unilateral in most cases, bilateral in <5% of cases.
- Undetected fluid-filled stomach below the diaphragm.
- Generally, abdominal circumference not significantly different from normative data.
- Thickened nuchal translucency at 10-14 weeks in nearly 40% of cases.
- MRI and CT amniography are helpful if obesity or fetal position make detection difficult.
- Three-dimensional ultrasound is helpful in the assessment of lung volume in cases of CDH, and is a potential predictor for pulmonary hypoplasia and postnatal outcome. The lung to head ratio may be a good predictor for fetal outcome.
- Main differential diagnoses include:
- Cystic adenomatoid malformation (intact diaphragm)
- Congenital hiatal hernia (midline dilated tubular structure)
- Pulmonary sequestration (intact diaphragm)
- Dextrocardia (unlike CHD, the apex points to the right)
- Lung tumor (dilated tubular structures).
- Right-sided hernia (<10% of cases):
- Right-sided chest mass, portal vein and gallbladder can be tracked within the mass
- The liver alignment is changed
- Pleural effusion is often seen on the same side
- The fluid-filled stomach is usually in a relatively normal location
- MRI is helpful in demonstration of the liver in the chest.
- Pitfalls:
- Despite high accuracy of sonographic diagnosis, a significant number of cases are missed. More than half are related to failure in following established guidelines.
- The classic sonographic features are not always present at the time of initial evaluation, therefore, CDH should be differentiated in all echogenic chest masses.
- Differentiating between congenital diaphragmatic eventration (better prognosis) and CDH may be very difficult.
- A collapsed bowel in the chest can easily be overlooked.
- Right-sided hernia is often more subtle.
- It may be confused with congenital hernia, a midline dilated tubular structure in the thoracic cavity.
- Lung changes are easily overlooked, especially if the stomach is in the abdomen.
- Diagnosable as early as 12 weeks for left-sided hernia and 17-18 weeks for right-sided hernia
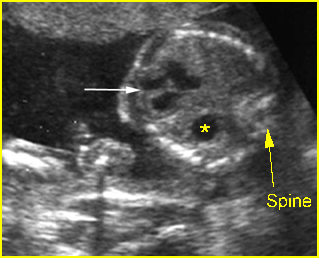
Fig 4: Pseudo-diaphragmatic hernia Oblique cross-sectional scan of the thorax: the stomach (*) seems to be located in the chest due to tangential scan (arrow = heart)
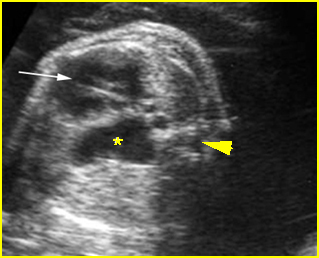
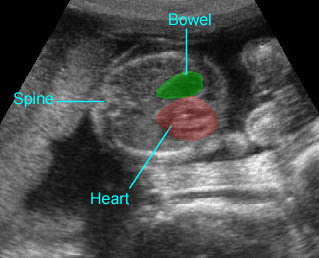
Fig 5: Diaphragmatic hernia Cross-sectional scan of thorax at the level of four-chamber view: cystic structure of bowel loop (*) located in the chest with cardiac displacement (arrow) to the right (arrowhead = spine)
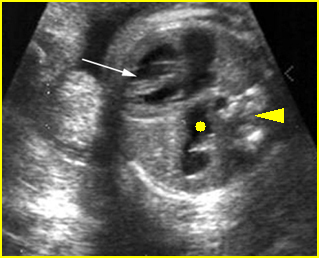
Fig 6: Diaphragmatic hernia Cross-sectional scan of thorax at the level of four-chamber view: cystic structure of bowel loop (solid circle) located in the chest with cardiac displacement to the right (arrowhead = spine)
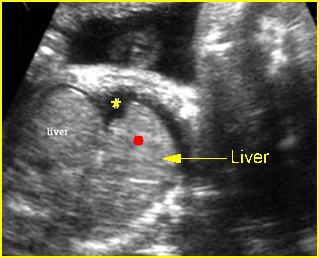
Fig 7: Right diaphragmatic hernia Sagittal scan of the chest: part of liver (solid circle) upward displacement to the chest (* = pleural effusion)
Video clips of diaphragmatic hernia
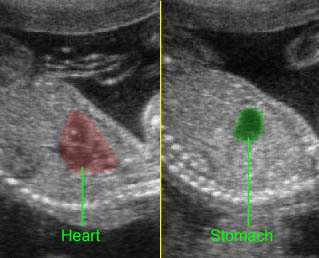
Diaphragmatic hernia: Sagittal scan: The stomach is herniated into the chest, next to the heart
Diaphragmatic hernia: Cross-sectional scan: The stomach is herniated into the chest, not seen in the abdomen, with cardiac displacement

Diaphragmatic hernia: Cross-sectional scan: The stomach is herniated into the chest with cardiac displacement
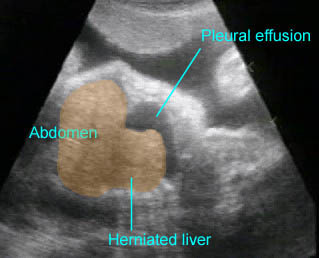
Right-sided diaphragmatic hernia: A portion of the liver herniated into the chest with pleural effusion
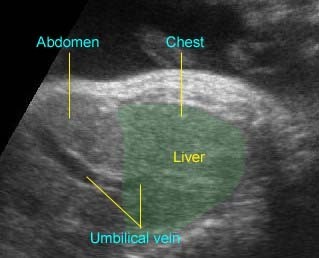
Right-sided diaphragmatic hernia: Right-sided diaphragmatic hernia: the liver herniated in the chest, the umbilical vein running into the chest
Associations: More than 25% had associated anomalies, including anomalies of the heart (20%), brain (30%), genitourinary system, craniofacial region, or limbs. Chromosomal abnormalities occur in 5-15%, with the most common being trisomy 18.
Management: In utero tracheal occlusion to promote lung growth in severe cases was impressive in preliminary studies but was not confirmed by later randomized control trial (RCT). Intrauterine repair should be at present considered as an investigational technique. Ex utero intrapartum treatment has been successful in a few cases. The delivery should be in a tertiary center. CDH needs effective immediate resuscitation and maintaining adequate gas exchange by mechanical ventilation and surgery is delayed until the respiratory status is stable. Postoperative extracorporeal membrane oxygenation (ECMO) is helpful in decreasing the mortality rate.
Prognosis: Poor; the main two poor prognostic factors are pulmonary hypoplasia and associated anomalies; better prognosis is reported for isolated cases with proper surgical correction, especially with ECMO treatment, as well as high-frequency ventilation, and antenatal steroids for lung maturity.
Recurrence risk: Usually sporadic with a low recurrence risk but a familial case with a higher risk for recurrence was found in <2% of cases.

