Normal Abdomen
Normal Examination
Routine screening often provides clues to the presence of a fetal GI disorder. Recognition of various signs such as ascites or intra-abdominal cysts, etc. requires a familiarity with the appearance of the structures normally found in the fetal abdomen. Guidelines proposed by the American Institute of Ultrasound in Medicine include five views of the abdominal structures: abdominal circumference, stomach, renal area, bladder, and cord insertion. These include the stomach, gallbladder, urinary bladder, and portal vein, etc. Routine evaluation of these structures can identify most fetuses with abdominal anomalies.
Axial scans:
- In general, the fetal abdomen has a round shape on axial scan. However, pressure from the uterine wall and fetal extremities often distorts the abdominal contour in late pregnancy.
- Abdominal circumference (AC): The AC is a measure of fetal girth, including soft tissue of the abdominal wall, as well as a measure of internal organs, primarily the liver. It is measured on an axial plane at the level of the stomach and the bifurcation of the main portal vein into the right and left branches. It should be as round as possible and in a perpendicular plane to the spine. Ribs should show a symmetric covering of the AC contours. The AC, although useful as an adjunctive parameter for fetal dating, is of greatest value in the evaluation of fetal growth in the latter part of pregnancy. Normal measurements of the liver, spleen, pancreas, stomach, gallbladder, and intestine have been established. Comprehensive reference ranges for first trimester fetal biometry have also been established. AC is the most important parameter in the estimation of fetal weight. However, careful measurement is always required. The accuracy is better among experienced sonographers. AC quality criteria and adherence to protocols and audit are important. Failure to meet quality criteria results in clinically significant errors.
- Pseudoascites: In early pregnancy, intra-abdominal organs are not clearly separated from the abdominal wall but near term, the echogenic rim of subcutaneous fat may be separated from intra-abdominal contents by a lucent band, sometimes called pseudoascites, which represents the musculature of the abdominal wall.
- Esophagus: The normal esophagus can be visualized in the thorax in the latter half of pregnancy when carefully sought. It can be observed as either two or more parallel echogenic lines.
- Stomach: In the fetal left upper quadrant, the fluid-filled stomach can be visualized in nearly all normal fetus from the beginning of the second trimester. It is round or oval on transverse scan and elongated on sagittal scan. If it is well distended, the fundus, body, antrum and incisura angularis (a notch at the lesser curvature between the body and antrum) can be identified. Failure to visualize the stomach after 14 weeks is suggestive of esophageal atresia.
- Small bowels: The small bowel is normally visualized as an ill-defined area of increased but relatively inhomogeneous echogenicity at the lower central abdomen. Additionally, it also undergoes continuous, active peristalsis throughout late pregnancy. Distinguishing small bowel from large bowel is possible after midpregnancy, and becomes more obvious with advancing gestational age. Individual segments of normal small bowel should not exceed approximately 7 mm in diameter or 15 mm in length and are usually considerably smaller than these values. The small bowel is often seen in active peristalsis and changes in configuration during real-time observation. Hyperechogenic bowel is potentially associated with medically significant outcomes, including multiple anomalies, fetal death, viral infection and aneuploidy.
- Large bowel: The colon appears as a continuous tubular structure located in the periphery, filled with hypoechoic meconium. It progressively enlarges with meconium from 3 to 5 mm at 20 weeks to up to 20 mm at term. By the middle of the third trimester, colonic haustra can be identified in nearly all fetuses. The colon exhibits far less peristalsis than the small intestine. Defecation in utero is a normal function. A normal range of fetal bowel (descending colon and rectum) diameters from the early second trimester of pregnancy onwards has been established.
- Spleen: The spleen can be seen in the left upper abdomen, posterior to the stomach and lateral and superior to the left kidney, separated from the lung by the hypoechoic band of the diaphragm. Although not always easily visualized, it can usually be seen throughout the second half of gestation. It is homogeneous in appearance and slightly less echogenic than the liver, similar to the kidney. The nomogram for fetal spleen dimensions has been established and may be useful in detecting growth disorders of the fetal spleen. Additionally, color Doppler and three-dimensional power Doppler ultrasound can facilitate the antenatal diagnosis of splenomegaly and can help to delineate the spleen from the similar-looking neighboring liver.
- Pancreas: The pancreas, although often overlooked, is sometimes visualized in the third trimester, especially with the fetus in a supine position. It lies posterior to the stomach and appears as a band of tissue with rather homogeneous echoes between the splenic and superior mesenteric artery.
- Liver: The liver is the dominant organ in the upper fetal abdomen, the area for standard abdominal circumference measurements. It spans the entire width of the abdomen throughout pregnancy. Except for anechoic vessels running through the parenchyma, the liver is homogeneous. The right lobe is all of the hepatic tissue lying to the right of the gallbladder middle hepatic vein, and inferior vena cava. Fetal liver measurements are usually obtained in a longitudinal plane, from the dome of the right hemidiaphragm to the tip of the right lobe. The liver progressively increases in size throughout a normal gestation. The normal range of fetal liver sizes for each week of pregnancy from 20 weeks of gestation to term has been established.
- Gallbladder: The gallbladder appears as a fluid-filled, teardrop-shaped structure inferior to the liver on the right. The length and width can be easily measured. Nonvisualization of the fetal gallbladder in early pregnancy is uncommon but is significantly associated with other fetal anomalies, for example extrahepatic biliary atresia.
- Hepatic veins converge near the superior central portion of the liver to join the inferior vena cava. In the same region, the ductus venosus can occasionally be identified on transverse scan forming a communication between the left portal vein and the inferior vena cava.
- The umbilical vein enters the mid-abdomen and courses superiorly near the anterior abdominal wall to the liver, where it turns posteriorly through the intersegmental fissure to terminate in the left portal vein. Two umbilical arteries join the umbilical vein at the umbilicus and just inferior to it. They arise from the iliac vessels bilaterally below the aortic bifurcation.
- Kidneys: The kidneys can usually be visualized in the late first trimester in more than 90% of cases. The kidneys appear on either side of the spine. At the beginning of the second trimester, they are sonolucent, and are round on transverse scans and bean-shaped on longitudinal scans. By midpregnancy, an echogenic outer rim of the renal capsule is seen. The central collecting system becomes echogenic toward the end of the second trimester as renal sinus fat develops. By the third trimester, hypoechoic medullary pyramids can be seen radiating from the renal sinus. The anteroposterior diameter of the renal pelvis is the simplest and most sensitive technique for prenatal diagnosis of congenital hydronephrosis, allowing identification of 100% of cases. Postnatal follow-up studies are warranted if the anteroposterior pelvic diameter on transverse scan is >4 mm before 33 weeks or >7 mm after 33 weeks. Throughout pregnancy, the ratio of the kidney circumference to the abdominal circumference remains relatively constant at 0.27-0.30. Nomograms of fetal renal size are established and may be useful in the evaluation of fetal growth restriction or renal pathology.
- Adrenal glands: The fetal adrenal glands, located superior to the upper renal poles, are often visualized when searching for the kidneys, especially in the third trimester. The gland characteristically has two long limbs that are relatively anechoic (thought to be the fetal zone of the cortex) and a central echogenic line in each limb (presumed medulla). They have a specific size, shape and echogenicity, appearing as hypoechoic crescents or chevrons with a faint echogenic band through the middle. The echo pattern is so characteristic that the cortex and medulla can be appreciated separately. Fetal adrenal gland volume, especially using 3D ultrasound, may be useful in prenatal diagnosis of congenital adrenal hyperplasia or fetal growth.
- Bladder: The bladder is a cystic intra-abdominal structure that can be seen from late first trimester. It is located between two echogenic iliac crests on transverse scan and fills the small fetal pelvis on sagittal scan. The bladder wall is thin and usually invisible when the bladder is distended. Changes in the volume of the bladder with time differentiate it from other pathologic cysts. The fetal urethra is usually invisible, however, it may occasionally be visualized as an echogenic line extending the length of an erect penis.
- Fetal gender: The external genitalia can usually be imaged from early in the second trimester onwards. Gender should always be determined in certain circumstance such as twins pregnancy, suspicion of lower urinary tract obstruction, fetal risk for X-linked disorders, etc. Male genitalia are readily seen. The penis and scrotum are most obvious. Testes may be seen in the scrotal sac, sometimes in the third trimester. Hydrocele, mostly insignificant, observed during pregnancy is common. Female gender should be assigned only by identification of the major and minor labia. Assigning female gender due to an inability to see a penis will result in many diagnostic errors. In approximately 3% of cases fetal gender is incorrectly assigned. This inaccuracy often is due to the fact that the labial hypertrophy during pregnancy may be misinterpreted as the male scrotum.
- Polyhydramnios: Although polyhydramnios can occur in a variety of disorders and is often a non-specific finding of unknown etiology, it is significantly related to GI obstruction.
- Oligohydramnios: Oligohydramnios, which is not secondary to fetal growth restriction or rupture of membrane, is often associated with urinary tract abnormalities.
Abdominal Wall
Visualization of cord insertion and the adjacent anterior abdominal wall must be included in routine obstetric scanning as recommended by the guidelines adopted by the American Institute of Ultrasound in Medicine. Normal cord insertion and the adjacent abdominal wall exclude the majority of abdominal wall defects.
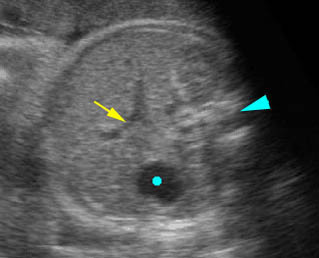
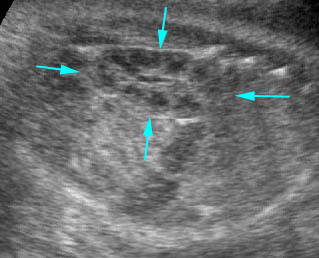
Fig 1: Normal fetal abdomen: Transverse scan: arrow = umbilical vein, solid circle = stomach, arrowhead = spine
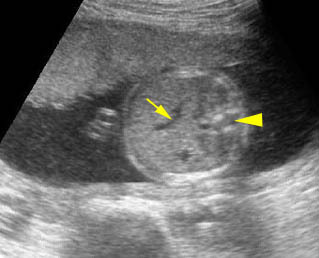
Fig 2: Normal fetal abdomen: Transverse scan: arrow = umbilical vein, arrowhead = spine
Video clips of normal fetal abdomen
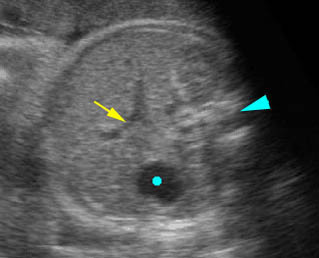
Normal fetal abdomen: Transverse scan: arrow = umbilical vein, solid circle = stomach, arrowhead = spine
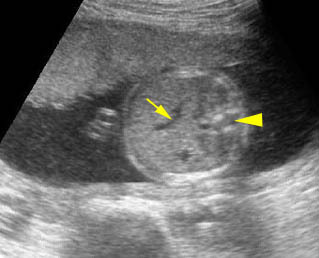
Normal fetal abdomen: Transverse scan: arrow = umbilical vein, arrowhead = spine
Normal kidney: Sagittal scan of the fetal kidney: arrows = outline of the kidney consisting of several hypoechoic pyramids

Female genitalia: Scan focus on the perineum: arrow = labia minora, * = bladder
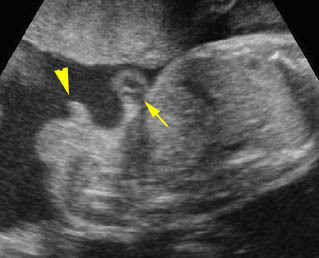
Male genitalia: From cross-section to mid-sagittal scan of the fetal trunk: arrow = cord insertion, arrowhead = penis
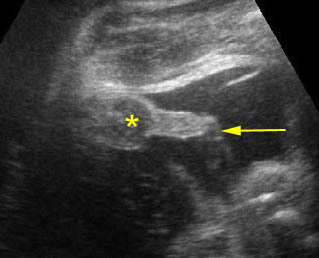
Male genitalia: Scan focus on the scrotum (*) and urinating penis (arrow)

Voiding: Male genitalia with urination
Technique
- On routine ultrasound examination in pregnancy, the demonstration of the abdominal cord insertion and the integrity of the anterior abdominal wall as well as the stomach and bladder must always be studied.
- The serial transverse scans from one end of the abdomen to the other end may be performed first and the fetal abdomen wall can be viewed continuously.
- On these serial scans, one should observe the smooth contour of the abdominal wall, normal cord insertion and umbilical location, fluid-filled stomach at the left upper abdomen, and fluid-filled urinary bladder at the mid-lower abdomen. It is extraordinarily important that cord insertion is imaged, due to the fact that many of the small omphaloceles which are often associated with chromosomal defects can easily be missed. The number of umbilical vessels can also be counted at the umbilicus. With color flow, both umbilical arteries at both sides of the bladder can be easily determined.
- On the inner aspect of the abdominal wall, a thin, 1-3 mm anechoic zone, representing the muscle tissue of the abdominal wall, runs continuous with the rib.
- Demonstration of the fetal abdominal wall may be very difficult in certain circumstances. For example, the extremities are tight to the abdominal wall, and the fetus may be in a prone position, especially when combined with oligohydramnios. In these situations, the location of the umbilicus, often invisible, may be assessed by identifying the umbilical vein in the upper abdomen and following it caudally until it approaches the abdominal wall and finally disappears from the abdomen. This point of disappearance should be at or just below the umbilicus.
- Sagittal views can also be helpful in following the umbilical vein and studying the contour of the abdominal wall. When possible, visualization of the proximal umbilical cord with enumeration of the vessels is ideal to rule out cystic lesions of the umbilical cord, such as a patent urachus.
- Fetal abdominal fat layer measurement may be useful for growth evaluation especially in diabetic mothers.
Checklists
On routine screening ultrasound, be sure that all of the followings are seen:
- Intact abdominal wall
- Fluid-filled stomach
- No ascites
- No abnormal mass
- Bladder
- Both kidneys with normal size, site and echogenicity
- Renal pelvis not dilated
- Bladder/ureter not dilated
- No renal cyst
- Normal amniotic fluid
Pitfalls
- Absent stomach: Inability to visualize the stomach in the second and third trimesters of pregnancy requires a repeated examination. About half of the cases will be proven to have a normal stomach on the repeated examination overtime (several hours or days later).
- Gastric pseudomass: A well-defined echogenic focus within the fetal stomach can normally be visualized in about 1% of sonographic evaluations. This is a pseudomass of cellular debris which mostly resolves spontaneously and should not be confused with an abnormality.
- Dilated colon: Unless correctly recognized, a normal enlarged colon is often mistaken for dilated small bowel, cysts or other pathological processes including renal cysts and pelvic masses. This potential pitfall is especially likely when the meconium, which is usually hypoechoic compared to the bowel wall, has a more sonolucent appearance.
- Spleen: The spleen is another upper abdominal organ that is often overlooked or mistaken for an abnormal solid left-sided mass.
- Gallbladder: The gallbladder is often overlooked or misrepresented sonographically (under the assumption that it represents an intrahepatic vein). Although it is a sonolucent structure, its ovoid/conical shape and lack of flow on Duplex or color Doppler, as well as its location inferior and to the right of the intrahepatic segment of the umbilical vein, should help distinguish it.
- Physiologic omphalocele: The bowel normally herniates into the proximal umbilical cord in the 8th gestational week but returns to the abdomen during the 12th week. However, the large herniated mass (>7 mm) regardless of gestational age should be considered abnormal.
- Pseudo-omphalocele: Oblique views of the fetus can give the false impression of an omphalocele, especially when the fetal limbs are tight to the abdomen and oligohydramnios. Compression of the fetal abdomen between the walls of the uterus or placenta can result in an appearance that mimics that of an omphalocele on sonography. This problem may simply be solved by obtaining all three proper planes. Furthermore, the differentiation can be made by demonstration of the thin covering membrane of the omphalocele, instead of a normal abdominal wall with subcutaneous fat in a pseudo-omphalocele.
- Pseudo-ascites: The thin anechoic zone of the fetal abdominal wall musculature which runs continuous with the rib can be mistaken for ascites. This anechoic zone is smooth and not crescent-shaped, as is ascites when bounded by bowel.
- A normal umbilical cord can be mistaken for gastroschisis especially when the umbilical cord is bunched and close to the abdomen. This problem can simply be solved by the demonstration of the flow with color Doppler. Nomograms of the umbilical cord and Wharton’s jelly area have been generated.
- Localized deposition of Wharton’s jelly at the umbilicus can be mistaken for a small omphalocele, but the mass is hyperechoic, not anechoic, as with bowel in an omphalocele, and the vessels run through it, not around it. Omphaloceles with predominately liver contents are also hyperechoic, but these defects are larger.
- A cystic mass near the cord insertion, such as omphalomesenteric cysts or allantoic cysts, may be confused with abdominal wall defects.

