Esophageal Atresia
This sporadic malformation results in an abrupt termination of the esophagus as a blind pouch. In approximately 90% of cases, esophageal atresia is associated with a tracheoesophageal fistula, which most often connects the trachea to the distal esophagus. Additional abnormalities occur in a high percentage of fetuses with esophageal atresia, and these include cardiac, chromosomal, gastrointestinal, genitourinary, and central nervous system lesions.
Incidence: About 1 in 3500 births, and nearly two-thirds are male.
Sonographic findings:
Fig 1, Fig 2, Fig 3
- Polyhydramnios: massive polyhydramnios (amniotic fluid index (AFI)>40) is commonly seen in the third trimester.
- Absent fluid-filled stomach in its normal location in the left upper quadrant.
- The absent visible stomach can be identified in about 42% of fetuses. Conversely, the combination of polyhydramnios and gastric non-visualization is only seen in less than half of fetuses with a tracheoesophageal fistula.
- Proximal esophageal pouch (pouch sign): a fluid-filled pouch corresponding to the atretic segment of the esophagus may be seen in the neck or distal esophageal segment.
- Fetal growth restriction: about 40% of infants with esophageal atresia are associated with growth restriction.
- Usually first diagnosable in the second trimester, mostly after 24 weeks.
- Among fetuses with ultrasonographic features suggestive of esophageal atresia, 50% have the disorder confirmed postnatally.
- In case of suspicion, MRI may be helpful.
- Pitfalls:
- Non-visualization of the stomach may be a transient normal finding.
- Several cases of tracheoesophageal fistula with a connection to the stomach through the lungs have a visible stomach.
- When combined with duodenal atresia, it may be very difficult to detect due to masking from polyhydramnios and double bubble sign.
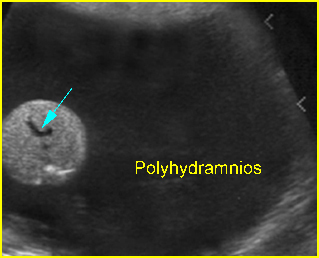
Fig 1: Esophageal atresia Cross-sectional scan of the abdomen: absent stomach at the level of umbilical vein complex (arrow) with marked polyhydramnios
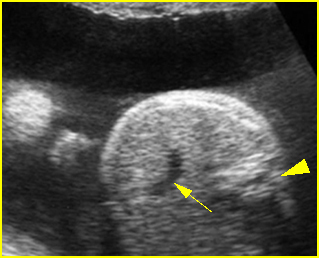
Fig 2: Esophageal atresia Cross-sectional scan of the abdomen: absent stomach at the level of umbilical vein complex (arrow) with polyhydramnios (arrowhead = spine)
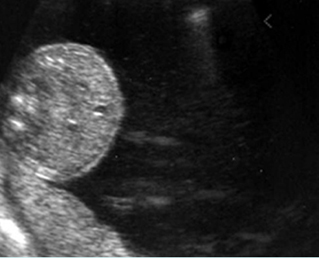
Fig 3: Esophageal atresia Cross-sectional scan of the abdomen: absent stomach with marked polyhydramnios
Video clips of esophageal atresia

Esophageal atresia: Cross-sectional scan of the abdomen: persistently absent stomach (arrow = umbilical vein, arrowhead = spine)
Associations: Associated malformations are seen in at least 50% of cases of tracheoesophageal fistula, including gastrointestinal, genitourinary, and cardiovascular anomalies, trisomy 21 and 18.
Management: A careful search for associated anomalies is indicated. The pregnancy with fetal isolated esophageal atresia should be closely followed-up and monitored for preterm delivery. The delivery should occur where appropriate personnel are available for surgical correction.
Prognosis: Poor overall (due to associated anomalies and prematurity), but the prognosis is much improved with isolated esophageal atresia.
Recurrence risk: Sporadic.

