Arachnoid Cysts
An arachnoid cyst is the accumulation of cerebrospinal-like fluid between the meninges, arising from the arachnoid separating into two layers. The cells lining the cyst wall produce CSF, which is trapped to form a cyst. The slipstreams of CSF within arachnoid cysts may not be channeled properly leading to possible damage of the surrounding brain parenchyma.
Incidence: Rare, sporadic occurrence, accounting for 1% of the intracranial lesions. Most are located above the tentorium and 5-10% occur in the posterior fossa. It has a male preponderance and increased incidence on the left side.
Sonographic findings:
- A well circumscribed, often circular fluid-filled space with a thin wall, located anywhere within the subarachnoid space.
- Usually displaces adjacent brain structures.
- Hydrocephalus secondary to a mass effect may be seen in some cases, however, most do not disturb normal brain function.
- The differential diagnosis for asymmetric cyst is porencephaly and for the midline cyst includes an interhemispheric cyst in the case of agenesis of the corpus callosum, Dandy-walker malformation, and dorsal sac of holoprosencephaly.
- MRI is helpful if the diagnosis is uncertain.
- Pitfalls:
- The cyst is sometime beneath the subcutaneous lesion mimicking meningocele.
- They may be missed if located in the portion of the brain closest to the transducer.
- Usually diagnosed in the second half of pregnancy, though may be detected as early as 13 weeks.
Associations: Rare.
Management: In general, isolated arachnoid cyst does not alter standard obstetric management.
Prognosis: Good, unless it is associated with other anomalies; most are asymptomatic, but they can cause neurological signs and symptoms, but good outcomes with neurosurgical intervention. Prenatal resolution can also occur.
Recurrence risk: Rare.
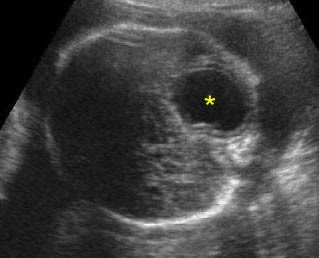
Arachnoid cyst: Transverse scan of the head: isolated cystic, circular, thin-walled brain lesion (*)
Vein of Galen Aneurysm
Vein of Galen aneurysm is dilatation of the vein ranging from a large single arteriovenous malformation to multiple smaller communications. It is a rare but pathognomonic midline intracranial cyst, located posterior and slightly superior to the thalami within the subarachnoid space.
Incidence: Unknown.
Sonographic findings:
- Well-defined midline tubular cyst just posterior and superior to thalami.
- Demonstration of the feeding vessels with arterial or venous flow by Doppler and color-flow study. Moreover, pulsation in the vein of Galen is also suggestive of fetal compromise and occurs earlier than those in umbilical vein.
- High-output congestive heart failure, polyhydramnios, hydrops fetalis, and sequele of the aneurysm may be seen in some cases.
- Three-dimensional color power angiography aids in visualization of the feeder vessels.
- Differential diagnoses
- interhemispheric cyst associated with agenesis of the corpus callosum
- arachnoid cyst
- dorsal sac associated with holoprosencephaly
- the diagnosis of vein of Galen aneurysms is rapidly established with color and pulsed Doppler.
- Pitfalls:
- A quadrigeminal cistern, a normal cystic structure posterior to the third ventricle, may be mistaken for the aneurysm, however, Doppler ultrasound will show no flow.
- Centrally placed arachnoid cyst can be confused with the aneurysm, however, Doppler ultrasound will show no flow.
- Usually first diagnosable in the third trimester, but possible as early as 14 weeks.
Associations: Most cases occur as isolated anomalies but cardiac defects, cystic hygroma and hydrocephalus may be seen in some cases. Pulmonary hypertension, and high-output heart failure or hydrops fetalis can be a consequence of the aneurysms.
Management: Termination of pregnancy may be offered, especially in the case of hydrops. In continuing pregnancies, serial sonographic monitoring to identify early signs of hydrops is indicated. Elective cesarean section when fetal lung maturity is attained may improve prognosis.
Prognosis: Poor in cases of heart failure or hydrocephalus, with numerous feeder vessels, a wide draining vein, and steal retrograde aortic flow; better in selected cases without suprasystemic pulmonary hypertension with appropriate surgical correction such as a staged endovascular technique or embolization. The malformations can also spontaneously disappear in rare cases.
Recurrence risk: Rare.
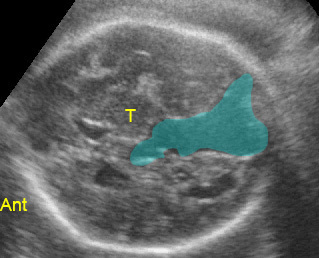
Aneurysm of vein of Galen: Midline tubular cystic space, predominantly located posteriorly (Ant: anterior; T: thalamus)
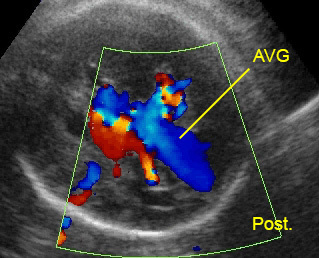
Aneurysm of vein of Galen (AVG): Midline tubular cystic space with circulating blood flow (Post: posterior)
Intracranial Hemorrhage In Utero
Fetal intracranial hemorrhage has rarely been observed. Such hemorrhage usually originates from germinal matrix with rupture into the ventricles. This may be due to the extreme capillary permeability of the vascular germinal matrix, which makes it susceptible to hemorrhage and often related to maternal factors, such as preeclampsia, or bleeding disorders. Germinal matrix or intraventricular hemorrhage is commonly classified in four grades as follows: Grade I: limited to subependymal matrix, Grade II: intraventricular extension, but without ventriculomegaly, Grade III: intraventricular extension, with ventriculomegaly, Grade IV: intraparenchymal extension.
Incidence: About 1 in 1000 pregnancies, very common in premature infants following delivery, may be as high as 40% among infants of <32 weeks.
Sonographic findings:
- The sonographic appearance varies with the location, size, and age of hemorrhage.
- An echogenic clot filling the ventricles followed by ventriculomegaly. Once the hemorrhage resolves, only ventriculomegaly may be evident.
- Hydrocephalus with mixed echogenic debris layering within the ventricles.
- Large hemorrhages may produce a marked mass effect.
- Subdural hematomas appear as echogenic or complex fluid collections just beneath the cranium, displacing and distorting the brain.
- Occasionally, mixed echogenic, enlarged choroid plexus results from hemorrhage into the choroid plexus.
- Porencephalic cyst following the hemorrhage may be seen.
- Mostly occurs in the beginning of the third trimester of pregnancy.
- The primary differential diagnosis includes intracranial neoplasm or infection.
- MRI is helpful for differentiating intracranial echogenicities suspected of hemorrhage.
Associations: No specific anomaly.
Prognosis: Depends on the extent of hemorrhage and intraparenchymal hemorrhage. The outcome is usually poor, especially for those fetuses affected by higher-grade intraventricular hemorrhages, whereas it is better in the subgroup with intraventricular hemorrhage.
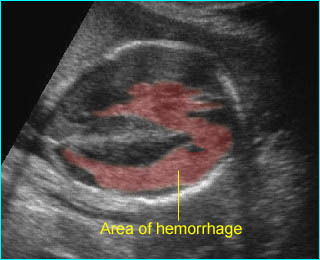
Intracerebral hemorrhage: Irregular echogenic mass in the area of lateral ventricle and cerebral mantle
Intracranial Neoplasms
Fetal intracranial neoplasms are rare and most occur in the perinatal period. Teratoma is the most common tumor detected antenatally, accounting for 62% of cases.
Incidence: Approximately 0.34 per 1 million live births.
Sonographic findings:
- Usually irregular in appearance.
- Mostly echogenic mass with occasional cystic portions with or without distortion of normal symmetrical intracranial structures, calcifications.
- Located anywhere within the brain.
- Craniomegaly, obstructive hydrocephaly seen in some cases.
- Associated polyhydramnios and hydrops fetalis occasionally seen.
- Infrequently abnormal cerebral Doppler flow velocimetry.
- Prenatal ultrasonography had high specificity in the diagnosis of brain neoplasms but the accuracy in predicting the histological type was limited.
- Most diagnosed in late second and third trimesters.
Association: No.
Management: Termination of pregnancy can be offered when diagnosed before viability.
Prognosis: Usually poor, though postnatal successful resection has been reported.
Recurrence risk: Rare.
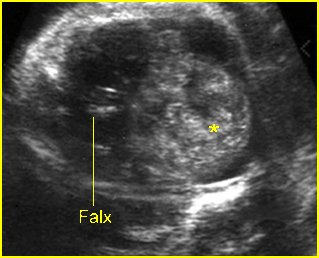
Fig 1: Fetal brain tumor Abnormal complex mass (*) with heterogeneous echo in the skull
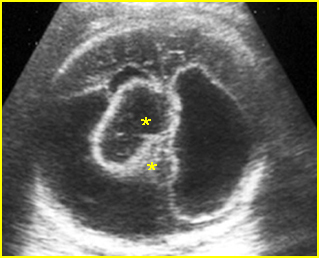
Fig 2: Ependymoma Complex cystic mass (*) in the skull combined with fluid collection and partial absence of brain tissue
Video clips of cerebral tumors
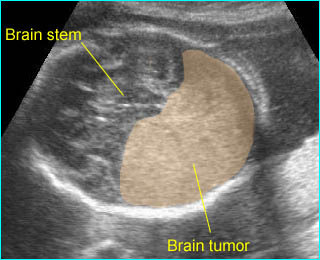
Solid brain tumor: Large homogeneous echogenic mass in the occipital region
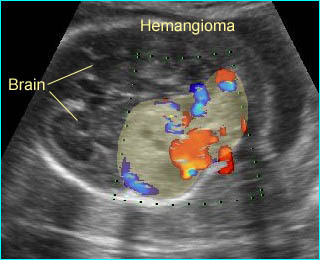
Hemangioma of subarachnoid: Complex solid-cystic mass in the occipital region with high vascularization

