Normal Examination
A systematic routine sonographic approach is necessary to minimize errors in detecting cerebral malformations. At least three standard axial views (transthalamic, transventricular, and transcerebellar views) should always be obtained as part of all obstetric ultrasound examinations during the standard second and third trimester examination. If abnormalities are suspected on these standard axial planes, then additional coronal and sagittal views may occasionally provide additional information.
Technique of examination
Fig1, Fig2, Fig3, Fig4, Fig5, Fig6, Fig7, Fig8, Fig9
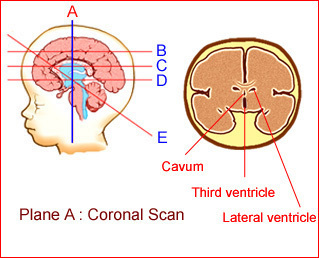
Fig1: Schematic drawing: Coronal view of the normal brain
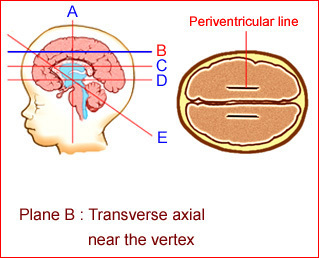
Fig 2: Schematic drawing: Transverse axial view near the vertex of the normal brain; note periventricular lines
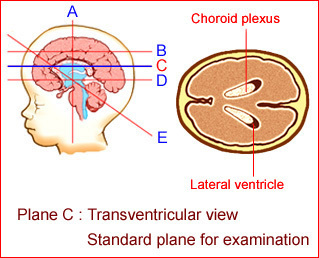
Fig 3: Schematic drawing: Normal transventricular view; the standard plane for assessment of the lateral ventricles
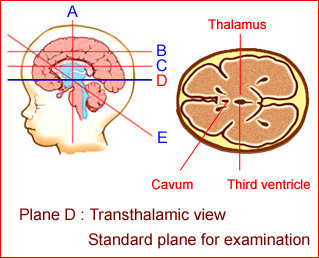
Fig 4: Schematic drawing: Normal transthalamic view; the standard plane for measurement of the biparietal diameter and head circumference
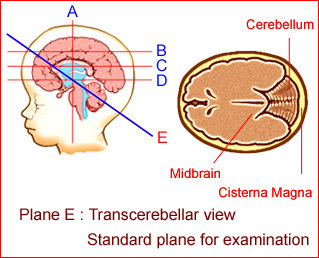
Fig 5:Schematic drawing: Normal transcerebellar view; the standard plane for assessment of the posterior fossa and occipital bone
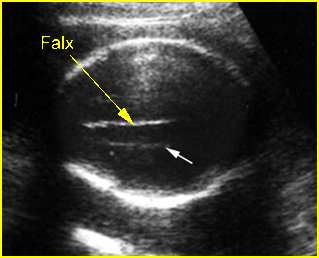
Fig 6:Periventricular line: Transverse scan of the skull at the higher level than transventricular view (arrow = periventricular line)
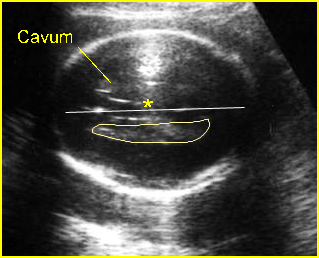
Fig 7:Transventricular view : Cross-sectional scan at the level of lateral ventricles; note: the lateral ventricle near the ultrasound transducer is usually obscure (in late pregnancy) secondary to reverbaration
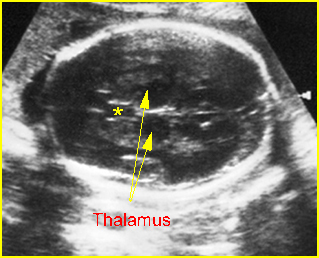
Fig 8:Standard plane of BPD measurement : Transverse scan of the head at the level of biparietal diameter (* = cavum septum pellucidum)
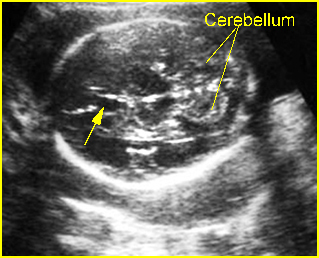
Fig 9: Normal cerebellum : Standard plane of transcerebellar examination (arrow = cavum septum pellucidum)
To obtain the three standard axial planes and their potential benefits, a systematic approach may be performed as follows:
- Slide, rock, tilt or rotate the transducer on the maternal abdomen to obtain the transaxial image of the fetal head and then move the transducer up to the top of the skull and gradually move down, keeping the transverse images symmetrical.
- Adjust the transducer to keep the ultrasound beam perpendicular to the anteroposterior diameter of the fetal skull.
- At the level superior to the transventricular view, the midline falx cerebri and bilateral periventricular lines, representing either deep intracerebral veins or periventricular white matter tract, should be visualized. The shape, echodensity and integrity of the cranium should also be observed.
- Keep moving the transducer down in the same manner, until the standard symmetrical transventricular plane is demonstrated. Meticulous inspection of this view is essential for early detection of hydrocephalus or choroid plexus cyst or other cerebral abnormalities.
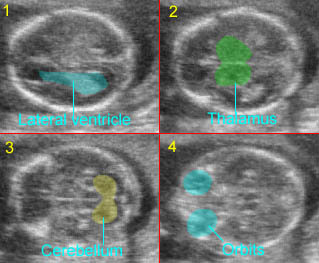
Normal fetal head Label On/Off
1) Lateral ventricles filled with choroid plexus; 2) Transthalamic view: plane for BPD measurement; 3) Transcerebellar view; 4) Biorbital view
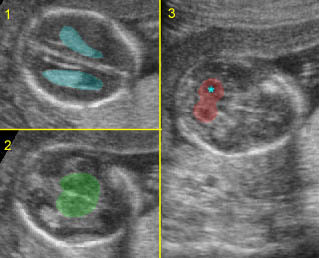
Standard planes:
1) Transventricular plane; 2) Transthalamic plane; 3) Transcerebellar standard plane: * = cerebellum
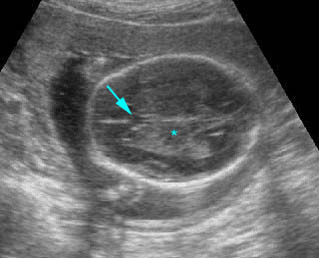
Transthalamic view: Transthalamic view for BPD and HC measurement; (* = thalamus, arrow = cavum septum pellucium)
Ventricular atrium measurement: The measurement is performed at the level of the glomus of the choroid plexus of the atrium distal to the ultrasound transducer. Calipers are positioned at the level of the glomus of the choroid plexus, inside the echoes generated by the walls of the ventricles. This diameter is relatively constant (4-8 mm with an upper limit of 10 mm; +3 SD) throughout the second and third trimesters. The male fetuses have slightly but significantly larger measurements of ventricular size than females.
– Keep moving the transducer down, until the standard transthalamic view just inferior to the level of the transventricular view is demonstrated. This is the standard plane used for obtaining the biparietal diameter and head circumference.
– A reverberation artifact from the skull table usually obscures the proximal hemisphere, however, changes in probe orientation may allow for subjective evaluation of the proximal hemisphere. A technique using an oblique scan plane angled superiorly through the temporal bone can improve visualization of the proximal hemisphere.
– Transthalamic view: The cavum septi pellucidi, a cerebrospinal fluid (CSF)-containing structure located between the frontal horns, must be visualized. With transabdominal ultrasound, it should always be visualized between 18 and 37 weeks or with a biparietal distance %BPD% of 44-88 mm. One should keep in mind that the absence of the cavum septi pellucidi is part of the malformations such as holoprosencephaly and agenesis of the corpus callosum. When scanning through this region, the shape of the cranium can also be assessed.
– Head measurements: BPD and head circumference %HC% measurement can be performed on the symmetrical transthalamic plane, and one should observe the ovoid skull shape, symmetrical bilateral thalami, cavum septum pellucidi, and the third ventricle which is located between thalami as a midline echo. BPD can be measured by placing calipers where the skull is broader using a gain set up so that the thickness of the parietal bones is <3 mm. The measurement is taken from the outer table of the proximal skull with the cranial bones perpendicular to the ultrasound beam to the inner table of the distal skull. The HC can be either directly measured or calculated from the BPD and occipitofrontal diameter (OFD) [HC=(BPD+OFD) x1.57].
– From the transthalamic level, rotate the transducer caudally to visualize the transcerebellar view, an angled view through the posterior fossa.
- Posterior fossa assessment: On the transcerebellar plane: the cerebellar hemispheres, cisterna magna and occipital bone should be demonstrated. The dumbbell-shaped cerebellum with slightly more echogenicity than the cerebrum is surrounded by CSF and is separated from supratentorial structures by the tentorium. The cisterna magna appears as a fluid space located between the dorsum of the cerebellar hemisphere and the occipital bone. The anteroposterior measurement of the cisterna magna obtained in the midline from the posterior margin of the cerebellar vermis to the inner wall of the occipital bone is about 3-10 mm. In the normal fetus, arachnoid septations typically are visualized within the cisterna magna. Finally, be sure that occipital bone is well intact. The transcerebellar view is important for the identification of small occipital cephaloceles, the Dandy-Walker variants and cerebellar signs of spina bifida.
If abnormalities are suspected on the standard axial planes examination then additional comprehensive examinations are helpful such as coronal and sagittal views, tissue harmonic imaging, MRI, 3D-US for brain volume measurement, and brain blood flow.
Checklist:
– Overview
- shape: normal, oval (no lemon, strawberry, cloverleaf, irregular shape secondary to compression in the presence of oligohydramnios)
- bone echodensity: normal
- calvarium: skull intact
– Transventricular view
- choroid plexi: free of cysts, and at a normal angle to midline
- cerebral ventricles: normal ventricular hemisphere ratio, normal size
– Transthalamic view
- normal biometry
- presence of the septum pellucidi
- third ventricle not dilated
– Transcerebellar view
- cerebellum: normal configuration (not banana), vermis intact
- cisterna magna: AP diameter <10 mm
- occipital bone intact
- nuchal soft tissues: measurement from the outer edge of the skull to the outer edge of the skin should be <6 mm.
Pitfalls
Pseudohydrocephalus
In the early second trimester of pregnancy, the cortical mantle on the side farthest from the transducer is relatively sonolucent compared to adjacent intracranial structures such as the subarachnoid, which may be misinterpreted as the lateral ventricular wall, causing further confusion. This confusion may be avoided by noting that
- There is a specular reflection anteriorly that represents the normal sylvian cistern and middle cerebral artery.
- Scanning more cephalad helps to visualize the true walls of the frontal horn of the lateral ventricle.
- Both the medial and lateral walls of the ventricular atrium can be recognized with meticulous scanning.
- The ventricular choroid plexus remains relatively parallel to the long axis of the lateral ventricle (absence of dangling choroid).
Unilateral hydrocephalus
Frequently, the upside fetal cerebral ventricle is not visualized due to acoustic noise by the bony calvarium in the near field and this can lead to the erroneous diagnosis of unilateral hydrocephalus. This artifact can be avoided by angling the transducer through the anterolateral fontanel or the thinner squamosal portion of the temporal bone to visualize the obscured fetal cerebral ventricle.
- The hemisphere nearest to the transducer is virtually always clouded over by reverberation artifacts generalized as acoustic beam passes through the near calvarial wall. The sonologist should assume that the intracranial anatomy of the fetus is symmetric, whether normal or abnormal, unless images document an asymmetry.
Choroid plexus pseudocyst
An oval hypoechoic structure can be visualized in the inferior and lateral aspect of the atrium of the lateral ventricle. This should not be mistaken for a true choroid plexus cyst. This artifact may be recognized based on its oval shape, small size, and constant location and by noting that the structure is without a strong acoustic interface (wall), which occurs with a true cyst.
Note:
- The fetal head can be clearly discriminated from the fetal torso when an embryo reaches a crown-rump length of 10-15 mm.
- By the end of the first trimester, the thalamus, third ventricle, midbrain, brain stem, and cerebellar hemispheres have achieved an appearance that will remain mostly unchanged, but with progressive enlargement.
- By 12-13 weeks, the lateral ventricles can be clearly seen, and they appear ovoid, are highly echogenic, and are largely filled with choroid plexus. Only the frontal horns are devoid of choroid plexus. The cerebral mantle surrounding the lateral ventricle is hypoechogenic.
- 13-15 weeks of gestation: the choroid plexus has a more normal posterior location; the anterior horns appear more prominent and are devoid of choroid plexus.
- 18-20 weeks of gestation: cavum septum pellucidum and posterior fossa can readily be evaluated and the cerebral mantle has thickened appreciably. The lateral ventricles have acquired their adult components, however, the size of the atria remains largely unchanged.
- Between 24 weeks and term, the brain undergoes little structural change other than increased cortical growth and the increase in convolutions. The increase in brain volume causes the lateral ventricles to become progressively less conspicuous.

