Agenesis of the corpus callosum
Agenesis of the corpus callosum (ACC), a bundle of white matter tracts decussating between the cerebral hemispheres, is related to several etiologic factors including genetic factors and is also a part of many syndromes.
Incidence: 0.3-0.7% of the general population and 2-3% of the developmental disabled.
Fig 1, Fig 2, Fig 3, Fig 4, Fig 5, Fig 6
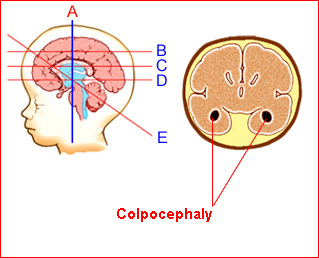
Fig 1: Schematic drawing: Coronal scan shows dilatation of the oc-cipital horn in agenesis of the corpus callosum (colpocephaly) (no interhemispheric cyst)
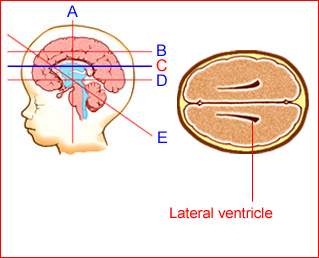
Fig 2: Schematic drawing: Both ventricular walls are identified where only periventricular lines are normally present.
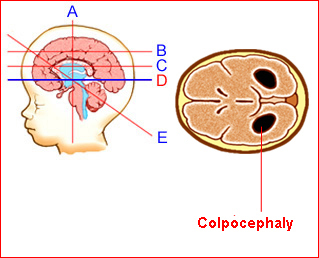
Fig 3: Schematic drawing: Transthalamic view shows characteristic dilatation of the occipital horns (colpocephaly)
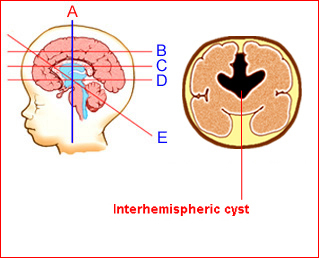
Fig 4: Schematic drawing: Coronal scan shows interhemispheric cyst in agenesis of the corpus callosum
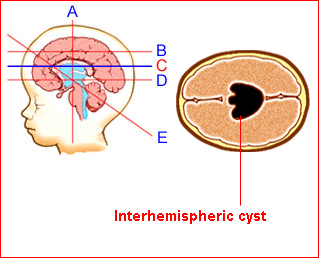
Fig 5: Schematic drawing: Transventicular view shows interhemispheric cyst in agenesis of the corpus callosum
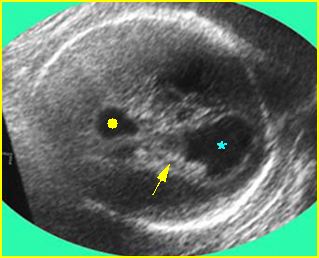
Fig 5: Colpocephaly: Transverse scan of the skull: dilated occipital horn of lateral ventricles (*), and third ventricle (solid circle) (arrow = choroid plexus)
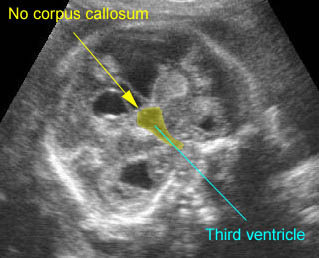
Sonographic findings
- The diagnosis is a challenge and sonographic findings are extremely variable.
- Demonstration of the absence of the corpus callosum by midcoronal and midsagittal scans (however, this is rather difficult).
- Failure to visualize the cavum septum pellucidum.
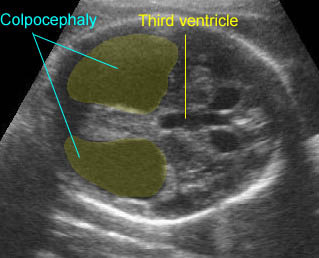
- Enlargement of the atria and occipital horns (colpocephaly).
- On routine transverse plane, separation of the bodies of the lateral ventricles resulting in the teardrop configuration of the lateral ventricles and a more parallel course of both ventricular walls than normal.
- Typically, enlargement and upward displacement of the third ventricle, forming an interhemispheric cyst.
- Reference ranges of the normal fetal corpus callosum dimensions have been available for objective assessment.
- When ACC is suspected, MRI is helpful in its confirmation.
- Differential diagnosis:
- lobar holoprosencephaly
- arachnoid cyst (usually not exactly midline)
- mild ventriculomegaly (entirely dilated ventricle)
- enlarged cavum septum pellucidum and cavum verga (the third ventricle will be in the normal position).
- Pitfalls: Development of the corpus callosum may not be complete until 18 weeks; therefore, the diagnosis on earlier examinations may be incorrect.
- Usually in the third trimester, but first diagnosable at about 18 weeks.
Agenesis of the corpus callosum: Transverse scan at the level of lateral ventricles: mild colpocephaly (solid circle) with interhemispheric cyst (*)
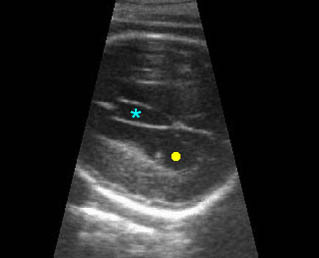
Agenesis of the corpus callosum: Ventriculomegaly with obviously prominent occipital horn (colpocephaly)
Agenesis of the corpus callosum: Coronal scan of the fetal brain showing the absence of the corpus callosum, just thin membrane above the third ventricle

Colpocephaly: Transverse scan of the head: bilateral marked dilatation of occipital horn (*) of lateral ventricles
Associations: Found in 50% of cases, most frequently DWM and cardiac defects, and chromosomal abnormalities, most frequently trisomy 18, are found in 20%. ACC may be part of several syndromes.
Management: In continuing pregnancies, a careful search for associated anomalies and postnatal follow-up is indicated. The delivery should occur in a tertiary center with full capabilities of diagnosis and management.
Prognosis: Depends on associated anomalies and the extent of agenesis; relatively good in isolated ACC, with an 85% chance of a normal developmental outcome and a 15% risk of handicap. Complete ACC has a worse prognosis than partial ACC.
Recurrence risk: Depends on the underlying specific disorder. Most isolated defects are sporadic.

