Cephalocele
Cephalocele is a protrusion of intracranial contents through a bony defect of the skull. Most cephaloceles are midline and occipital extracranial masses. If only meninges protrude, it is called meningocele. Cephaloceles may be a part of several syndromes, especially Meckel syndrome (cephalocele, polycystic kidneys, and polydactyly) or trisomy 13, and are often associated with other malformations.
Incidence: 1-5 in 10,000 births, which varies with ethnic group and geographic region. Occipital cephaloceles are most common in the West, whereas anterior cephaloceles are much more common in Southeast Asia (1:5000 in Thailand compared with 1:35,000-40,000 in Europe).
Sonographic findings:
Fig 1, Fig 2, Fig 3, Fig 4
- Skull defect, usually in the occipital area (90% of cases), best visualized on the standard transcerebellar and transthalamic view.
- Skull defect of anterior cephalocele is more difficult to visualize and may present as extracranial mass with hypertelorism and the cephalocele may best be seen on the facial profile view.
- Skull defect in an asymmetric area is often related to amniotic band syndrome and other associated anomalies may be seen.
- Extracranial mass protruding through the defect
- meningocele, an entirely cystic mass
- a solid mass, often showing gyri and sulci (encephalocele)
- a solid cystic mass (meningoencephalocele).
- Microcephaly, commonly seen.
- Possibly ventriculomegaly.
- Polyhydramnios in some cases.
- The lemon-shaped appearance of the bony calvarium that occurs with open NTD and with the Arnold-Chiari type II malformation.
- Associated anomalies of specific syndrome, especially Meckel syndrome (cephalocele, polycystic kidneys, and polydactyly) , Waker-Warburg syndrome (cephalocele, ocular malformations, Dandy-Walker malformations), and Joubert syndrome.
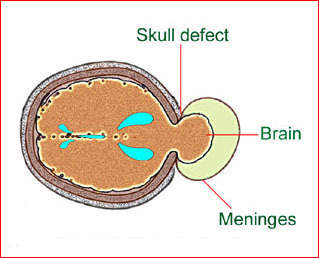
Fig 1: Schematic drawing: Occipital meningocele, protrusion of the brain tissue and meninges through the skull defect
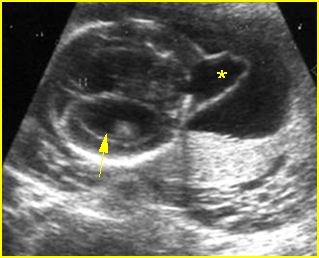
Fig 2: Occipital cephalocele Transverse scan of the skull: small defect of occipital bone with meningocele (*) (arrow = ventriculomegaly)
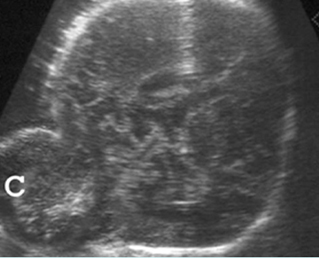
Fig 3: Occipital cephalocele Transverse scan of the skull: defect of occipital bone with meningoencephalocele (C)
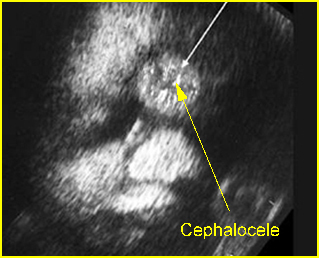
Fig 4: Anterior cephalocele Coronal scan of the face: round solid mass above the nose (arrow)
Video clips of cephalocele
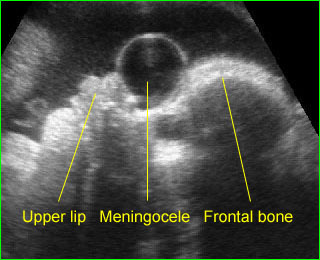
Anterior meningocele: Sagittal scan of the fetal face: frontal bone defect with midline cystic mass (meningocele)
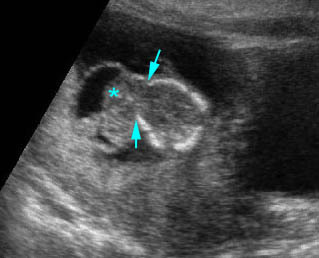
Anterior cephalocele: Transverse scan of the head: frontal skull defect (arrow) with protrusion of brain and meninges (*)
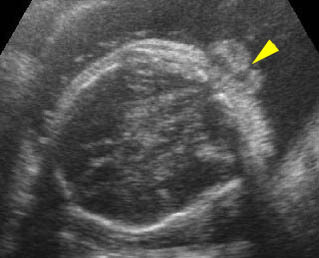
Occipital cephalocele: Transverse scan the level of cerebellum: small defect of occipital bone with encephalocele
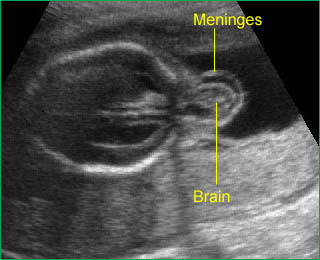
Occipital cephalocele: Transverse scan of the head: occipital skull defect with meningoencephalocele and mild ventriculomegaly
- Pitfalls:
- A scalp hemangioma, cephalhematoma, epidermal scalp cyst, caput succedaneum, or even the normal fetal ear can be mistaken for a cephalocele.
- The primary differential diagnosis of occipital cephaloceles includes
- cystic hygroma (most common); usually septate, cystic, no skull defect, often related to hydrops fetalis
- cervical meningocele
- cervical teratoma
- cranial hemangioma
- iniencephaly (very rare).
- Usually diagnosable after 11-14 weeks (transvaginal ultrasound) .
Associations: Ventriculomegaly (most common), Meckel syndrome, amniotic band syndrome, and limb-body wall complex, chromosome abnormalities (14% of cases).
Management: Termination of pregnancy can be offered for a severe case diagnosed before viability. For the less severe form, a careful search for other anomalies and karyotyping is indicated. The fetus should be delivered and have surgical correction in a tertiary center. A cesarean section could improve the prognosis by avoiding birth trauma and contamination of brain tissue with vaginal bacteria.
Prognosis: Poor in most cases, but good for small, cystic isolated meningocele. Neurological outcome depended on the occurrence or not of hydrocephalus, while the intelligence level was mainly related to the absence of cerebral tissue within the sac.
Recurrence risk: About 2-4%. Periconceptional folic acid supplementation can significantly decrease the recurrent risk.

