Dandy-Walker Malformation
Dandy-Walker Malformation (DWM)
DWM is characterized by a posterior fossa cyst, a defect of the cerebellar vermis, resulting in a communication between the cyst and the fourth ventricle, and variable hydrocephalus. It is one of the most common midline cysts located within the posterior fossa. DWM represents marked genetic and etiologic heterogeneity. It can be subdivided into two subgroups: classic DWM (dilated fourth ventricle with absence of the cerebellar vermis) and DWM variant (partial absence of the cerebellar vermis with a small posterior fossa cyst).
Incidence: 1 per 30,000 births, occurring in 3.5-12% of cases of hydrocephalus.
Sonographic findings:
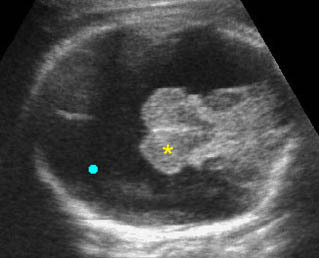
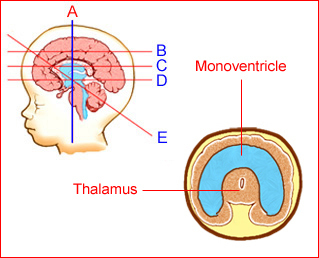
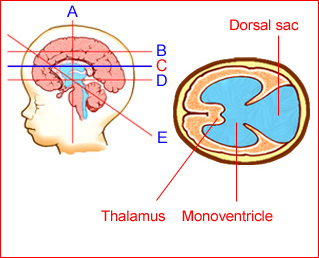
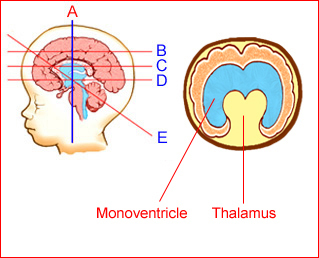
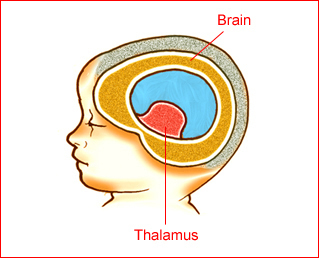
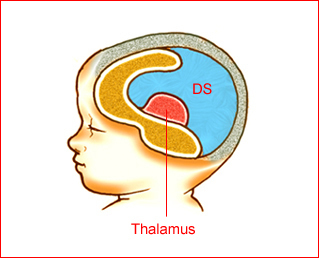
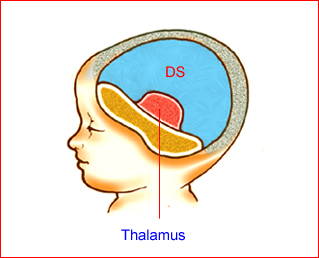
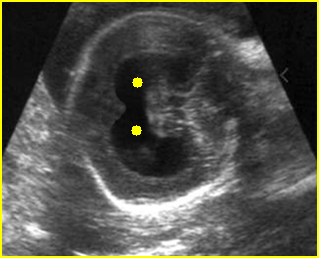
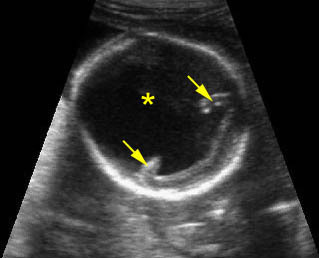
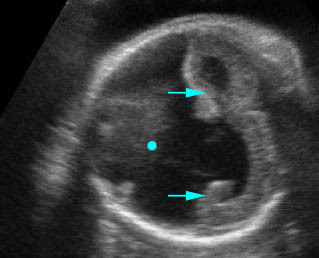
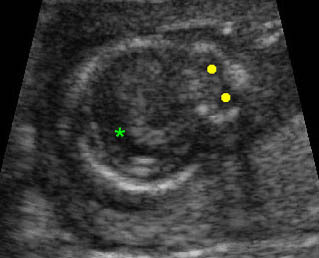
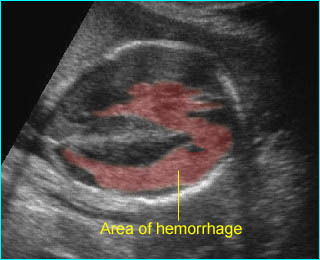
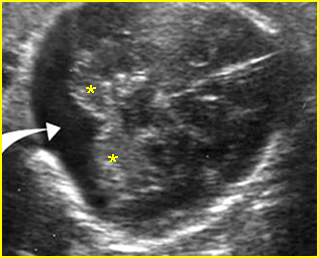
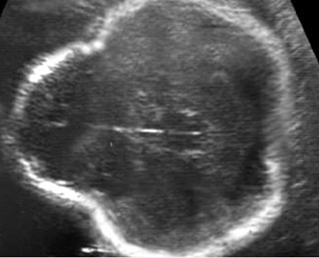
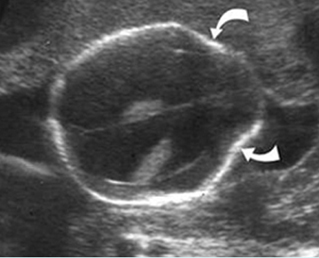
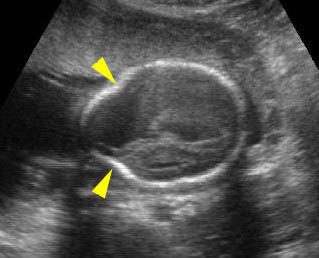
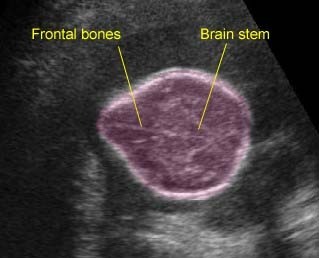
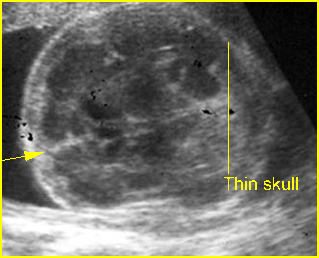
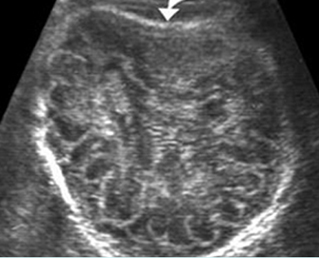
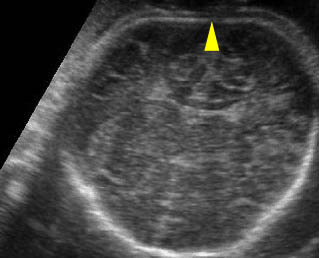
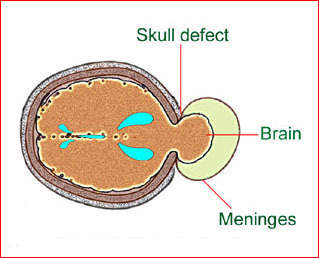
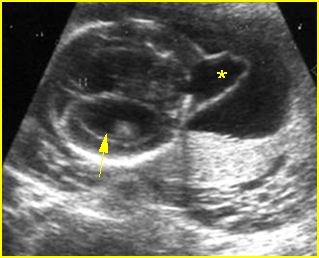
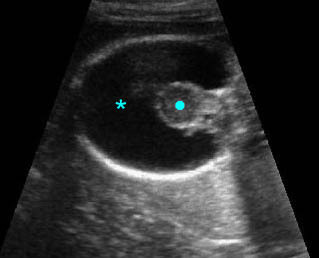
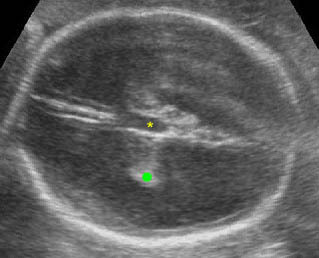
Fig 1, Fig 2, Fig 3
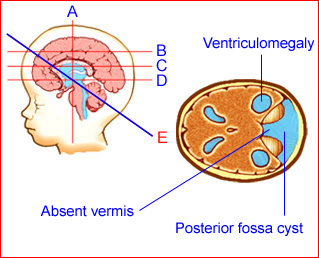
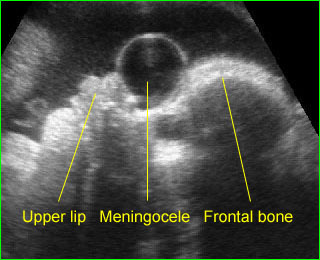
Fig 1: Schematic drawing: Posterior fossa cyst with absent cerebellar vermis in Dandy-Walker malformation
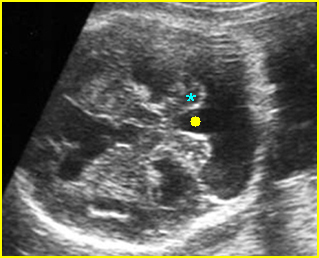
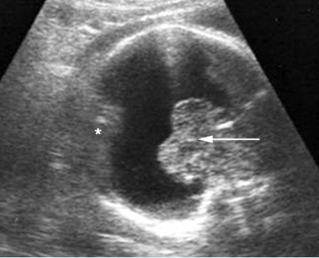
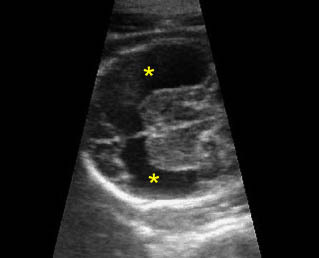
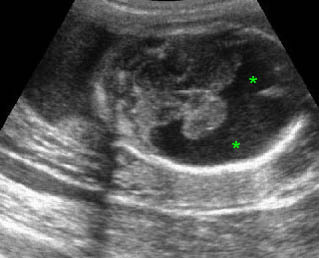
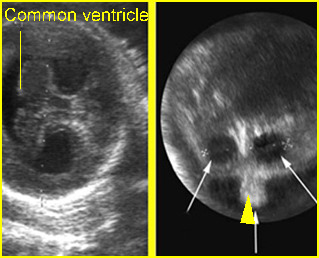
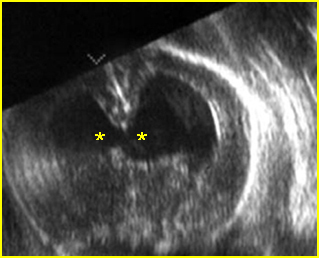
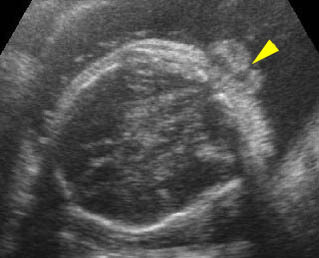
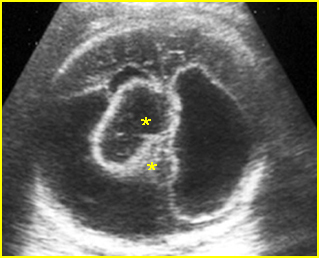
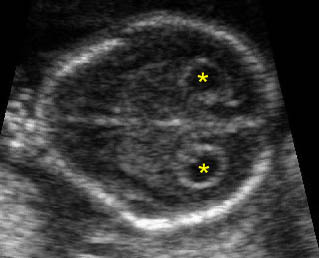
Fig 2: Dandy-Walker malformation Transcerebellar view: posterior fossa cyst, separation of cerebellar hemisphere (*), absent vermis (solid circle)
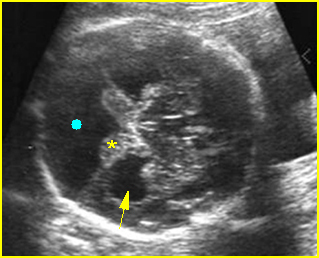
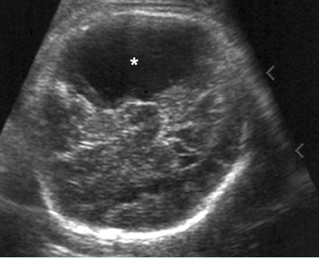
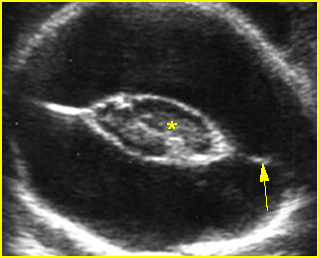
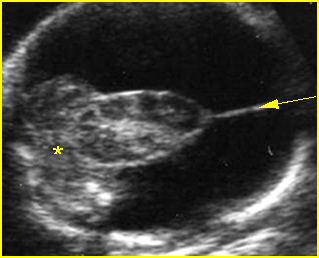
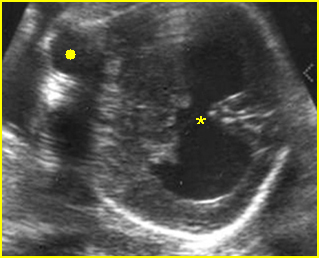
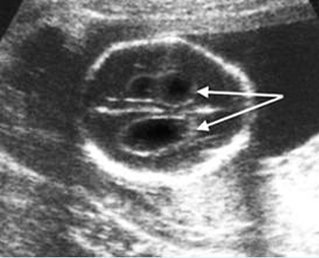
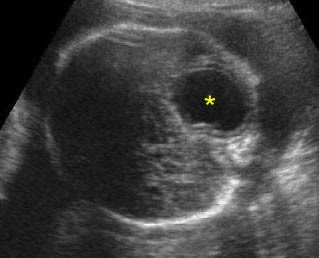
Fig 3: Dandy-Walker malformation Transcerebellar view: posterior fossa cyst (solid circle), separation of cerebellar hemisphere (*), absent vermis (arrow = associated ventriculomegaly)
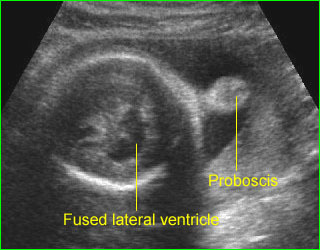
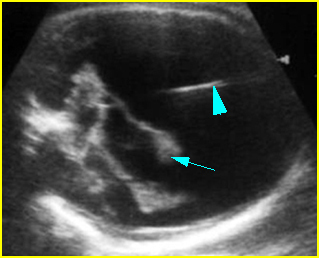
- Partial or complete absence of the cerebellar vermis (the direct continuity of the posterior fossa cyst with the posterior aspect of the midbrain can be visualized without an intervening vermis).
- Midline posterior fossa cyst caused by an enlargement of the fourth ventricle, communicating with cisterna magna.
- Splaying of the cerebellar hemispheres.
- Measurement of cisterna magna of more than 10 mm in classic DWM but normal in DWM variant.
- Classic DWM is associated with ventriculomegaly (30-80% of cases) but DWM variant is not.
- The main differential diagnosis is arachonoid cyst, usually not located in the midline and not associated with absent vermis.
- Pitfalls:
- An enlarged cisterna magna of >10 mm, but with a normally formed cerebellum is often mistaken for DWM variant.
- Isolated enlargement of the fourth ventricle at 14-16 weeks in the absence of vermian changes may be a normal variant.
- A small cyst inferior to the cerebellum is often a normal variant.
- Cerebellar hemorrhage followed by a porencephalic cyst of the cerebellum may mimic the classic form of Dandy-Walker malformation.
- Usually diagnosed in the second half of pregnancy, although it has been detected as early as the first trimester.

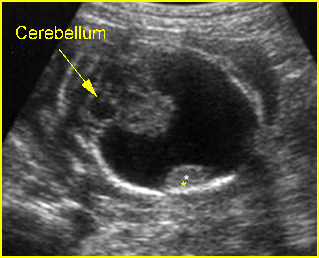
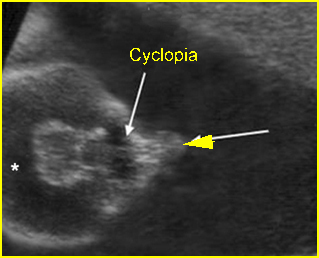
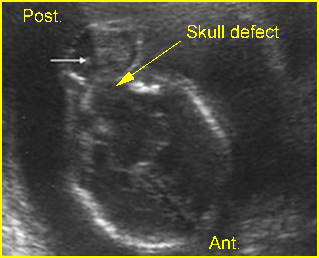
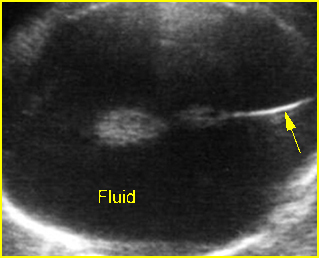
Dilated cisterna magna: Transcerebellar view: dilated cisterna magna (*)
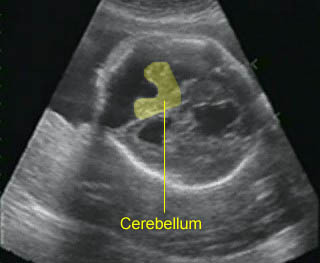
Dandy-Walker malformation: Cystic dilatation of the posterior fossa with separation of the cerebellar hemisphere and the absence of the vermis
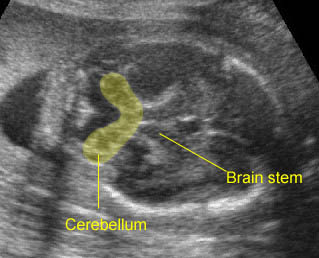
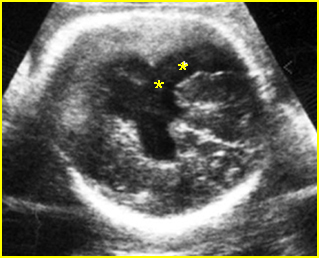
Dandy-Walker malformation: Separation of the cerebellar hemisphere and the absence of the vermis
Associations: Associated intracranial anomalies are found in about 50% of cases and associated extracranial anomalies in about 35%. Chromosome abnormalities are seen in about 15-30%, especially trisomy 18. DWM is also associated with several other chromosome abnormalities and several syndromes and is X-link recessive in some cases.
Management: Termination of pregnancy may be offered when diagnosed for classic DWM before viability. In continuing pregnancies, a careful search for associated anomalies and postnatal follow-up is indicated. Early delivery may be considered when there is progressive and severe hydrocephalus.
Prognosis: High morbidity and mortality rate, mostly related with other anomalies, but good for DWM variant without associated anomalies.
Recurrence risk: About 1-5% for an isolated case.