21-23 กันยายน 2563
กรุณาลงทะเบียนโดยกรอกข้อมูลในไฟล์ exel แล้วส่ง submit ทาง e-mail ที่: mfm.cmu@gmail.com
Please register Fetal Echo X (using the downloaded form from the link above and sending via e-mail: mfm.cmu@gmail.com

โครงการอบรมเชิงปฏิบัติการ
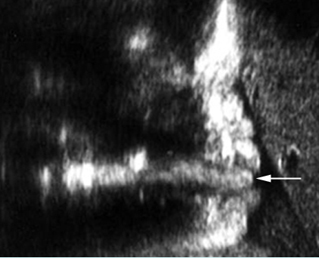
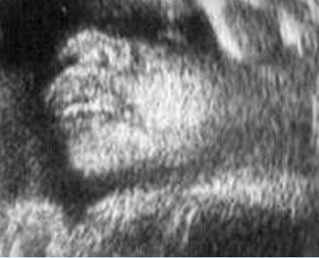
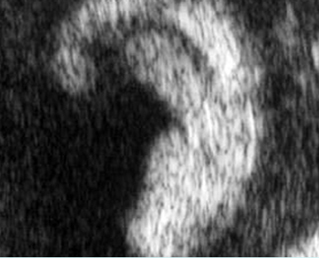
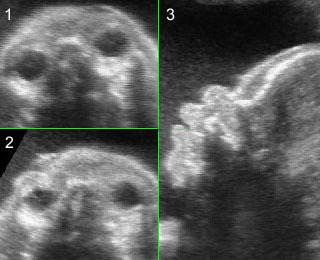
“การตรวจโรคหัวใจทารกในครรภ์ด้วยอัลตราซาวด์”
Fetal Echocardiography XI: Practical Points


วันที่ 22-23 กันยายน 2563
ณ ห้องประชุมชั้น 15 อาคารสุจิณโณ
คณะแพทยศาสตร์ มหาวิทยาลัยเชียงใหม่
1. หลักการและเหตุผล
ปัญหาสำคัญในการวินิจฉัยก่อนคลอดของโรคหัวใจพิการโดยกำเนิดสำหรับทารกในครรภ์ นับเป็นหนึ่งในเรื่องร้อนที่ท้าทาย (hot issue) ในสาขาวิชาเวชศาสตร์มารดาและทารก เนื่องจากเป็นความพิการโดยกำเนิดที่พบได้บ่อยที่สุด มีความชุกถึงประมาณร้อยละ 1 ของการคลอด เป็นสาเหตุสำคัญของการตายปริกำเนิดที่สัมพันธ์กับภาวะพิการโดยกำเนิดบ่อยที่สุดเช่นเดียวกัน และเป็นความพิการโดยกำเนิดที่พลาดจากการวินิจฉัยก่อนคลอดได้บ่อยที่สุด ทีมงานเวชศาสตร์มารดาและทารก ภาควิชาสูติศาสตร์และนรีเวชวิทยา คณะแพทยศาสตร์ มหาวิทยาลัยเชียงใหม่ ได้ทำการศึกษาค้นคว้าด้านการวินิจฉัยก่อนคลอดของโรคหัวใจพิการโดยกำเนิด (fetal echocardiography) อย่างต่อเนื่องมากว่า 20 ปี(1-57) และเป็นศูนย์กลางการฝึกอบรมแพทย์ต่อยอดเฉพาะทางเวชศาสตร์มารดาและทารก ได้เล็งเห็นความสำคัญของการมีทักษะในด้านนี้ ซึ่งนอกเหนือจากการมีประสบการณ์ ทักษะ ความคุ้นเคย และมีหลักการในการตรวจค้นหาอย่างเป็นระบบแล้ว ยังจำเป็นต้องมีการศึกษาต่อยอดอย่างต่อเนื่อง แบ่งปันประสบการณ์ เทคนิค และปรับตัวเรียนรู้ไปตามวิทยาการและเทคโนโลยีด้านนี้อย่างต่อเนื่อง ทางทีมงานมีความคาดหวังที่จะช่วยกันส่งเสริมความรู้และทักษะเชิงลึกด้านการตรวจหัวใจทารกในครรภ์ ให้มีประสิทธิภาพมากยิ่งขึ้น เพื่อการวินิจฉัยก่อนคลอดและวางแผนการดูแลรักษาตั้งแต่อายุครรภ์ยังน้อย หรือส่งตัวผู้ป่วยไปสู่การดูแลรักษาในสถานที่ที่มีความพร้อมมากกว่าเป็นต้น หรือแม้แต่การให้โอกาสทางเลือกในการยุติการตั้งครรภ์ตั้งแต่อายุครรภ์ยังน้อย (สำหรับรายที่ทารกมีความพิการชนิดรุนแรงที่อาจไม่สามารถมีชีวิตรอดได้) ดังนั้นทีมงานจึงได้จัดการประชุมวิชาการด้าน “การตรวจอัลตราซาวด์หัวใจทารกในครรภ์ : fetal echocardiography” อย่างต่อเนื่อง ในการจัดประชุมครั้งนี้จะเน้นเทคนิค เคล็ดลับสำคัญในการตรวจ เพื่อการวินิจฉัยโรคหัวใจทารกในครรภ์อย่างถูกต้อง และมั่นใจ ซึ่งเป็นการประยุกต์เทคโนโลยีที่มีอยู่ทั่วไปให้เกิดประโยชน์สูงสุด โดยมุ่งหวังให้ผู้เข้ารับการฝึกอบรมเพิ่มพูนทักษะการประยุกต์ใช้ให้มีความสามารถในการวินิจฉัยโรคหัวใจพิการโดยกำเนิดได้ก่อนคลอดด้วยความมั่นใจสูง รวมทั้งฟื้นฟูความรู้และเทคนิคในการตรวจใหม่ ๆ ของระบบหัวใจและหลอดเลือดซึ่งมีความก้าวหน้าไปอย่างรวดเร็ว และเนื่องจากทักษะสำคัญของการวินิจฉัยคือการตรวจหัวใจทารกในครรภ์ ซึ่งต้องอาศัยทักษะสูงกว่าการตรวจทั่วไป และแลกเปลี่ยนความรู้ในเชิงลึกของศาสตร์ด้านนี้กับผู้มีประสบการณ์
2. วัตถุประสงค์ เพื่อให้ผู้เข้ารับการอบรม
เพื่อเพิ่มทักษะ อัพเดตความรู้ และแลกเปลี่ยนประสบการณ์ในการตรวจวินิจฉัยหัวใจทารกในครรภ์ และ ตรวจวินิจฉัยโรคหัวใจพิการโดยกำเนิดให้ได้เร็วขึ้น โดยคาดหวังว่าผู้ฝึกอบรมสามารถวินิจฉัยโรคหัวใจพิการโดยกำเนิดตั้งแต่ระยะเริ่มแรก และสามารถประยุกต์ใช้อัลตราซาวด์ในการคัดกรองและวินิจฉัยหัวใจทารกผิดปกติได้อย่างมีระบบด้วยความมั่นใจมากขึ้น
3. ผู้เข้าร่วมโครงการ
3.1 วิทยากร 11 คน
3.2 สูติแพทย์ แพทย์ต่อยอดสาขาเวชศาสตร์มารดาและทารก และผู้สนใจ 60 คน
3.3 แพทย์ประจำบ้านสาขาสูติศาสตร์และนรีเวชวิทยา คณะแพทยศาสตร์ มหาวิทยาลัยเชียงใหม่ 60 คน
3.4 เจ้าหน้าที่ 6 คน
รวม 127 คน
4. วิทยากร
4.1 รองศาสตราจารย์ นายแพทย์วัชระ จามจุรีรักษ์
4.2 ศาสตราจารย์ นายแพทย์ธีระ ทองสง
4.3 รองศาสตราจารย์ นายแพทย์ชเนนทร์ วนาภิรักษ์
4.4 ศาสตราจารย์ แพทย์หญิงสุพัตรา ศิริโชติยะกุล
4.5 รองศาสตราจารย์ ดร. นายแพทย์วีรวิทย์ ปิยะมงคล
4.6 รองศาสตราจารย์ แพทย์หญิงเฟื่องลดา ทองประเสริฐ
4.7 รองศาสตราจารย์ แพทย์หญิง เกษมศรี ศรีสุพรรณดิฐ
4.8 รองศาสตราจารย์ แพทย์หญิงสุชยา ลือวรรณ
4.9 ผู้ช่วยศาสตราจารย์ แพทย์หญิงกุณฑรี ไตรศรีศิลป์
4.10 ผู้ช่วยศาสตราจารย์ นายแพทย์ ภูดิศ เจต๊ะวรรณ
4.11 อาจารย์ แพทย์หญิง ศิรินาถ ศิริเลิศศ
5. สถานที่
ห้องประชุมชั้น 15 อาคารสุจิณโณ คณะแพทยศาสตร์ มหาวิทยาลัยเชียงใหม่
6. ระยะเวลา
วันที่ 26-27 กันยายน 2562
7. ผู้รับผิดชอบโครงการ
หน่วยเวชศาสตร์มารดาและทารก ภาควิชาสูติศาสตร์และนรีเวชวิทยา
คณะแพทยศาสตร์ มหาวิทยาลัยเชียงใหม่
8. การลงทะเบียน
ลงทะเบียนโดยไม่เก็บค่าลงทะเบียน
9. งบประมาณ
9.1 ประมาณการรายรับ
• ได้รับการสนับสนุนจากโครงการวิจัยพัฒนาศักยภาพการวิจัยเชิงสถาบัน 100,000.- บาท
9.2 ประมาณการรายจ่าย
• ของที่ระลึกวิทยากร 3,000.- บาท
• ค่าอาหารว่างและอาหารกลางวัน 60,000.- บาท
• ค่าเอกสารและซีดีมัลติมีเดียประกอบการอบรม (130.- x 130 ชุด) 30,000.- บาท
• ค่าแผ่นพับ (10.- x 500 แผ่น) 5,000.- บาท
• ค่าแสตมป์และซองจดหมาย 2,000.- บาท
รวม 100,000.- บาท
10. ผลที่คาดว่าจะได้รับ
ผู้ฝึกอบรมสามารถประยุกต์ใช้อัลตราซาวด์ ในการตรวจประเมินโครงสร้างและการทำงานของหัวใจทารกในครรภ์ได้อย่างเป็นระบบและมีความมั่นใจมากขึ้น และสามารถวินิจฉัยก่อนคลอดของโรคหัวใจพิการโดยกำเนิดตั้งแต่อายุครรภ์ยังน้อยด้วยความมั่นใจมากขึ้น
11. เอกสารอ้างอิง
- Tongsong T, Srisomboon J, Wanapirak C, Sirichotiyakul S, Pongsatha S, Polsrisuthikul T. Pregnancy outcome of threatened abortion with demonstrable fetal cardiac activity: a cohort study. J Obstet Gynaecol (Tokyo 1995) 1995;21:331-5.
- Tongsong T, Wanapirak C, Sirichotiyakul S. Placental thickness at mid-pregnancy as a predictor of Hb Bart’s disease. Prenat Diagn 1999;19:1027-30.
- Tongsong T, Wanapirak C, Sirichotiyakul S, Piyamongkol W, Chanprapaph P. Fetal sonographic cardiothoracic ratio at midpregnancy as a predictor of Hb Bart disease. J Ultrasound Med 1999;18:807-11.
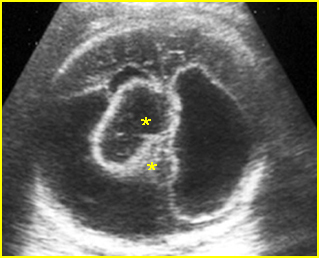
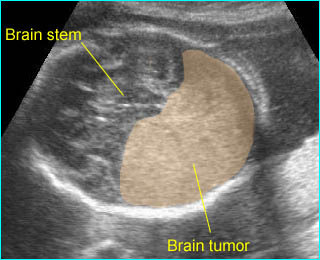
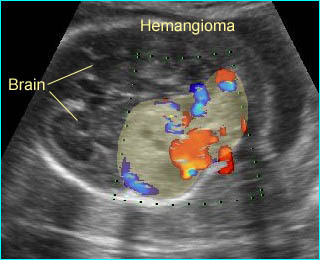
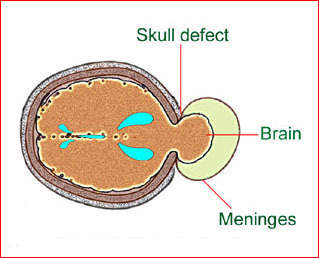
- Tongsong T, Sirichotiyakul S, Sittiwangkul R, Wanapirak C. Prenatal sonographic diagnosis of cardiac hemangioma with postnatal spontaneous regression. Ultrasound Obstet Gynecol 2004;24:207-8.
- Tongsong T, Sirichotiyakul S, Sukpan K, Sittiwangkul R. Prenatal features of a truncus arteriosus with pulmonary atresia and pulmonary circulation derived from the ductus arteriosus. J Ultrasound Med 2004;23:1221-4.
- Tongsong T, Sittiwangkul R, Wanapirak C, Chanprapaph P. Prenatal diagnosis of isolated tricuspid valve atresia: report of 4 cases and review of the literature. J Ultrasound Med 2004;23:945-50.
- Tongsong T, Tatiyapornkul T. Cardiothoracic ratio in the first half of pregnancy. J Clin Ultrasound 2004;32:186-9.
- Tongsong T, Wanapirak C, Sirichotiyakul S, Chanprapaph P. Sonographic markers of hemoglobin Bart disease at midpregnancy. J Ultrasound Med 2004;23:49-55.
- Tongsong T, Chanprapaph P, Khunamornpong S, Sirichotiyakul S. Sonographic features of Ebstein anomaly associated with hydrops fetalis: a report of two cases. J Clin Ultrasound 2005;33:149-53.
- Tongsong T, Chanprapaph P, Sittiwangkul R, Sirichotiyakul S. Rupture of fetal ductus arteriosus aneurysm. Obstet Gynecol 2005;105:1275-8.
- Tongsong T, Iamthongin A, Wanapirak C, Piyamongkol W, Sirichotiyakul S, Boonyanurak P, et al. Accuracy of fetal heart-rate variability interpretation by obstetricians using the criteria of the National Institute of Child Health and Human Development compared with computer-aided interpretation. J Obstet Gynaecol Res 2005;31:68-71.
- Tongsong T, Khunamornpong S, Wanapirak C, Sirichotiyakul S. Prenatal sonographic diagnosis of truncus arteriosus associated with holoprosencephaly. J Clin Ultrasound 2005;33:193-6.
- Tongsong T, Sittiwangkul R, Khunamornpong S, Wanapirak C. Prenatal sonographic features of isolated hypoplastic left heart syndrome. J Clin Ultrasound 2005;33:367-71.
- Tongsong T, Sittiwangkul R, Wanapirak C, Sirichotiyakul S. Prenatal diagnosis of transposition-like double-outlet right ventricle with mitral valve atresia in heterotaxy syndrome. J Clin Ultrasound 2005;33:197-200.
- Piyamongkol W, Trungtawatchai S, Chanprapaph P, Tongsong T. Comparison of the manual stimulation test and the nonstress test: a randomized controlled trial. J Med Assoc Thai 2006;89:1999-2002.
- Tongsong T, Chanprapaph P, Sittiwangkul R, Khunamornpong S. Antenatal diagnosis of double outlet of right ventricle without extracardiac anomaly: a report of 4 cases. J Clin Ultrasound 2007;35:221-5.
- Srisupundit K, Piyamongkol W, Tongsong T. Identification of fetuses with hemoglobin Bart’s disease using middle cerebral artery peak systolic velocity. Ultrasound Obstet Gynecol 2009;33:694-7.
- Tongsong T, Tongprasert F, Srisupundit K, Luewan S. High fetal splenic artery peak velocity in fetuses with hemoglobin Bart disease: a preliminary study. J Ultrasound Med 2009;28:13-8.
- Tongsong T, Tongprasert F, Srisupundit K, Luewan S. Venous Doppler studies in low-output and high-output hydrops fetalis. Am J Obstet Gynecol 2010;203:488.e1-6.
- Tongsong T, Tongprasert F, Srisupundit K, Luewan S. The complete three-vessel view in prenatal detection of congenital heart defects. Prenat Diagn 2010;30:23-9.
- Jatavan T, Luewan S, Tongsong T. Outcomes of pregnancy complicated by heart disease at Maharaj Nakorn Chiang Mai Hospital. J Med Assoc Thai 2011;94:1159-63.
- Luewan S, Tongprasert F, Piyamongkol W, Wanapirak C, Tongsong T. Fetal liver length measurement at mid-pregnancy among fetuses at risk as a predictor of hemoglobin Bart’s disease. J Perinatol 2011;31:157-60.
- Luewan S, Yanase Y, Tongprasert F, Srisupundit K, Tongsong T. Fetal cardiac dimensions at 14-40 weeks’ gestation obtained using cardio-STIC-M. Ultrasound Obstet Gynecol 2011;37:416-22.
- Tongprasert F, Srisupundit K, Luewan S, Sirichotiyakul S, Piyamongkol W, Wanapirak C, et al. Reference ranges of fetal aortic and pulmonary valve diameter derived by STIC from 14 to 40 weeks of gestation. Prenat Diagn 2011;31:439-45.
- Tongsong T, Piyamongkol W, Tongprasert F, Srisupundit K, Luewan S. Fetal splenic artery peak velocity (SPA-PSV) at mid-pregnancy as a predictor of Hb Bart’s disease. Ultraschall Med 2011;32 Suppl 1:S41-5.
- Tongsong T, Wanapirak C, Piyamongkol W, Sirichotiyakul S, Tongprasert F, Srisupundit K, et al. Fetal ventricular shortening fraction in hydrops fetalis. Obstet Gynecol 2011;117:84-91.
- Traisrisilp K, Tongprasert F, Srisupundit K, Luewan S, Tongsong T. Reference ranges for the fetal cardiac circumference derived by cardio-spatiotemporal image correlation from 14 to 40 weeks’ gestation. J Ultrasound Med 2011;30:1191-6.
- Luewan S, Srisupundit K, Tongprasert F, Tongsong T. Normal reference ranges of inferior vena cava doppler indices from 14 to 40 weeks of gestation. J Clin Ultrasound 2012;40:214-8.
- Tongprasert F, Srisupundit K, Luewan S, Wanapirak C, Tongsong T. Normal reference ranges of ductus venosus Doppler indices in the period from 14 to 40 weeks’ gestation. Gynecol Obstet Invest 2012;73:32-7.
- Jatavan T, Tongsong T. Comparison of fetal cardiac spatiotemporal image correlation segmental analysis between cardiac- and body-based scrolling. J Ultrasound Med 2013;32:2125-9.
- Luewan S, Tongprasert F, Srisupundit K, Tongsong T. Fetal myocardial performance (Tei) index in fetal hemoglobin Bart’s disease. Ultraschall Med 2013;34:355-8.
- Mekjarasnapha M, Traisrisilp K, Luewan S, Srisupundit K, Tongprasert F, Tongsong T. Reference ranges for fetal septum primum excursion from 14 to 40 weeks’ gestation. J Ultrasound Med 2013;32:1729-34.
- Siwawong W, Tongprasert F, Srisupundit K, Luewan S, Tongsong T. Fetal cardiac circumference derived by spatiotemporal image correlation as a predictor of fetal hemoglobin Bart disease at midpregnancy. J Ultrasound Med 2013;32:1483-8.
- Tongsong T, Luewan S, Srisupundit K, Jatavan T. Hemodynamic assessment of indomethacin-induced fetal heart failure in high-output state. J Clin Ultrasound 2013;41:438-40.
- Traisrisilp K, Tongprasert F, Srisupundit K, Luewan S, Tongsong T. Reference ranges of ductus arteriosus derived by cardio-spatiotemporal image correlation from 14 to 40 weeks of gestation. Gynecol Obstet Invest 2013;76:25-31.
- Luewan S, Tongprasert F, Srisupundit K, Tongsong T. Inferior vena cava Doppler indices in fetuses with hemoglobin Bart’s hydrops fetalis. Prenat Diagn 2014;34:577-80.
- Luewan S, Tongprasert F, Srisupundit K, Traisrisilp K, Tongsong T. Reference ranges of myocardial performance index from 12 to 40 weeks of gestation. Arch Gynecol Obstet 2014;290:859-65.
- Thathan N, Traisrisilp K, Luewan S, Srisupundit K, Tongprasert F, Tongsong T. Screening for hemoglobin Bart’s disease among fetuses at risk at mid-pregnancy using the fetal cardiac diameter to biparietal diameter ratio. BMC Pregnancy Childbirth 2014;14:230.
- Tongprasert F, Srisupundit K, Luewan S, Tongsong T. Comparison of cardiac troponin T and N-terminal pro-B-type natriuretic peptide between fetuses with hemoglobin Bart’s disease and nonanemic fetuses. Prenat Diagn 2014;34:864-9.
- Luewan S, Tongprasert F, Srisupundit K, Tongsong T. Fetal cardiac Doppler indices in fetuses with hemoglobin Bart’s disease at 12-14weeks of gestation. Int J Cardiol 2015;184:614-6.
- Tongsong T, Tongprasert F, Srisupundit K, Luewan S, Traisrisilp K. Cardio-STIC (spatio-temporal image correlation) as genetic ultrasound of fetal Down syndrome. J Matern Fetal Neonatal Med 2015;28:1943-9.
- Traisrisilp K, Tongprasert F, Srisupundit K, Luewan S, Sukpan K, Tongsong T. Prenatal differentiation between truncus arteriosus (Types II and III) and pulmonary atresia with ventricular septal defect. Ultrasound Obstet Gynecol 2015;46:564-70.
- Jatavan P, Kemthong W, Charoenboon C, Tongprasert F, Sukpan K, Tongsong T. Hemodynamic studies of isolated absent ductus venosus. Prenat Diagn 2016;36:74-80.
- Jatavan P, Tongprasert F, Srisupundit K, Luewan S, Traisrisilp K, Tongsong T. Quantitative Cardiac Assessment in Fetal Tetralogy of Fallot. J Ultrasound Med 2016;35:1481-8.
- Sirilert S, Tongprasert F, Srisupundit K, Luewan S, Tongsong T. Fetal septum primum excursion (SPE) and septum primum excursion index (SPEI) as sonomarkers of fetal anemia: using hemoglobin Bart’s fetuses as a study model. Prenat Diagn 2016;36:680-5.
- Srisupundit K, Tongprasert F, Luewan S, Traisrisilp K, Jatavan P, Tongsong T. Effect of cordocentesis on fetal myocardial performance. Prenat Diagn 2016;36:871-4.
- Tongsong T, Luewan S, Jatavan P, Tongprasert F, Sukpan K. A Simple Rule for Prenatal Diagnosis of Total Anomalous Pulmonary Venous Return. J Ultrasound Med 2016;35:1601-7.
- Tongsong T, Tongprasert F, Srisupundit K, Luewan S, Traisrisilp K. Ventricular Diastolic Function in Normal Fetuses and Fetuses with Hb Bart’s Disease Assessed by Color M-Mode Propagation Velocity using Cardio-STIC-M (Spatio-Temporal Image Correlation M-Mode). Ultraschall Med 2016;37:492-6.
- Traisrisilp K, Charoenkwan P, Tongprasert F, Srisupundit K, Tongsong T. Hemodynamic assessment of hydrops foetalis secondary to transient myeloproliferative disorder associated with foetal Down syndrome: A case report and literature review. J Obstet Gynaecol 2016;36:861-4.
- Tongprasert F, Sittiwangkul R, Jatavan P, Tongsong T. Prenatal Diagnosis of Aortopulmonary Window: A Case Series and Literature Review. J Ultrasound Med 2017;36:1733-8.
- Tongprasert F, Srisupundit K, Luewan S, Traisrisilp K, Jatavan P, Tongsong T. Fetal isovolumetric time intervals as a marker of abnormal cardiac function in fetal anemia from homozygous alpha thalassemia-1 disease. Prenat Diagn 2017;37:1028-32.
- Wanapirak C, Sirichotiyakul S, Luewan S, Srisupundit K, Tongprasert F, Tongsong T. Appearance of Abnormal Cardiothoracic Ratio of Fetuses with Hemoglobin Bart’s Disease: Life Table Analysis. Ultraschall Med 2017;38:544-8.
- Jatavan P, Chattipakorn N, Tongsong T. Fetal hemoglobin Bart’s hydrops fetalis: pathophysiology, prenatal diagnosis and possibility of intrauterine treatment. J Matern Fetal Neonatal Med 2018;31:946-57.
- Rueangdetnarong H, Sekararithi R, Jaiwongkam T, Kumfu S, Chattipakorn N, Tongsong T, et al. Comparisons of the oxidative stress biomarkers levels in gestational diabetes mellitus (GDM) and non-GDM among Thai population: cohort study. Endocr Connect 2018;7:681-7.
- Tongprasert F, Sittiwangkul R, Lerthiranwong T, Tongsong T. Prenatal sonographic monitoring of progressive cardiac damages caused by anti-Ro antibodies: A case report. J Clin Ultrasound 2018;46:347-50.
- Tongsong T, Tongprasert F, Srisupundit K, Luewan S, Traisrisilp K, Jatavan P. Fetal Cardiac Remodeling in Response to Anemia: Using Hemoglobin Bart’s Disease as a Study Model. Ultraschall Med 2018.
- Sirilert S, Tongprasert F, Srisupundit K, Tongsong T, Luewan S. Z Score Reference Ranges of Fetal Cardiothoracic Diameter Ratio. J Ultrasound Med 2019;38:999-1007.

ตารางกำหนดการประชุม
Pre-Seminar course: วันจันทร์ที่ 21 กันยายน 2563: 9.00-16.00 น. โดยคณาจารย์
Pre-conference Course: โดยคณาจารย์
- Cardiac Embryology (8.30-10.00 น.) : นพ. ธีระ ทองสง
- The benefits of Colour M-mode in a normal fetal heart (10.00-10.30) : นพ. วัชระ จามจุรีรักษ์
- Standard cardiac exam (10.45-12.00 น.) : พญ. สุพัตรา ศิริโชติยะกุล
- Physics of ultrasound (13.00-14.00 น.) : นพ. ธีระ ทองสง
- Image optimization (ปรับภาพ) (14.00-15..00 น.) : พญ. สุชยา ลือวรรณ
- Hands-on live demonstration : พญ. สุชยา ลือวรรณ นพ. ธีระ ทองสง นพ. วัชระจามจุรีรักษ์
{tabulizer:style[gr.alterora.elemental_1_yellow_green.css]}
| วันอังคารที่ 22 กันยายน 2563 |
| 08.15 – 08.45 น. |
ลงทะเบียน – Spot Diagnosis |
ศ. นพ. ธีระ ทองสง |
| 08.45 – 09.00 น. |
Opening Ceremony |
คณบดี / หัวหน้าภาควิชาฯ |
| 09.00 – 10.00 น. |
Right heart anomaly |
ศ. พญ. สุพัตรา ศิริโชติยะกุล |
| 10.00 – 10.15 น. |
———————-พัก———————– |
|
| 10.15 – 11.00 น. |
Tip & Tricks XI : 3VV-3VT view |
ศ. นพ. ธีระ ทองสง |
| 11.00 – 12.00 น. |
Cardiac function : Brain-heart relationship |
ผศ. ดร. นพ. ภูดิศ เจต๊ะวรรณ |
| 12.00 – 13.00 น. |
———รับประทานอาหารกลางวัน———- |
|
| 13.00 – 13.45 น. |
First trimester scan |
รศ. พญ. สุชยา ลือวรรณ |
| 13.45 – 14.30 น. |
Amazing five-chamber view |
ศ. นพ. ธีระ ทองสง |
| 14.30 – 14.45 น. |
———————-พัก———————– |
|
| 14.45 – 15.45 น. |
Genetic aspect of congenital heart |
ผศ. พญ. กุณฑรี ไตรศรีศิลป์ หมื่นพินิจ |
| 15.45 – 16.30 น. |
Case presentation I: Echo-patho correlation |
อ. พญ. ศิรินาถ ศิริเลิศ / รศ. พญ. กรกนก สุขพันธ์ |
{tabulizer:style[gr.alterora.elemental_1_orange.css]}
| วันพุธที่ 23 กันยายน 2563 |
| 08.15 – 9.15 น. |
Case presentation II |
เฟลโล่ / ทีมงาน |
| 09.15 – 10.15 น. |
DORV/TGA/TOF |
รศ. พญ. สุชยา ลือวรรณ |
| 10.15 – 10.30 น. |
———————-พัก———————– |
|
| 10.30 – 11.00 น. |
Truncus arteriosus |
ศ นพ. ธีระ ทองสง |
| 11.00 – 12.00 น. |
Fetal heart failure |
รศ. พญ. เกษมศรี ศรีสุพรรณดิฐ |
| 12.00 – 13.00 น. |
———รับประทานอาหารกลางวัน———- |
|
| 13.00 – 14.00 น. |
Arrhythmia I |
รศ. พญ. เฟื่องลดา ทองประเสริฐ |
| 14.00 – 14.45 น. |
Arrhythmia II |
รศ. พญ. เฟื่องลดา ทองประเสริฐ |
| 14.45 – 15.00 น. |
———————-พัก———————– |
|
| 15.00 – 15.45 น. |
Left heart anomalies |
ศ. นพ. ธีระ ทองสง |
| 15.45 – 16.15 น. |
Bizarre clip quiz |
รศ. นพ. ชเนนทร์ วนาภิรักษ์ |
| 16.15 – 16.30 น. |
Closing Ceremony |
ร.ศ. พ.ญ. พรรณี ศิริวรรธนาภา/รศ. นพ. ชเนนทร์ วนาภิรักษ์ |