Omphalocele
Omphalocele is a defect in the anterior abdominal wall with extrusion of abdominal contents in the base of the umbilical cord. The herniated mass is covered by parietal peritoneum and amnion, with Wharton’s jelly intervening between the two membrane layers.
Fig 1, Fig 2
Incidence: 1 in 3000-4000 births with a male to female ratio of about 1:5. An increased incidence has been observed with advancing maternal age.
Sonographic findings:
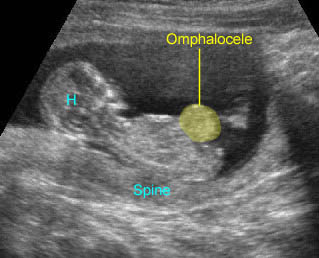
- Typically, a midline mass with a covering membrane adjacent to the abdominal wall containing abdominal contents (bowel or liver). Eighty percent of cases contain liver, sometimes with small bowel. The stomach and bladder may occasionally lie in the omphalocele. Fig 3, Fig 4, Fig 5, Fig 6, Fig 7
- Variable depending on the amount of ascites, degree of herniation and associated anomalies.
- Twenty percent contain gut and fluid only and most abnormal chromosomes are seen in this subgroup.
- Omphaloceles containing bowel alone tend to be small and can be missed or mistaken for gastroschisis. Fig 8
- Umbilical cord inserting on the sac.
- Ascites commonly seen.
- The covering membrane may not always be seen, particularly in the absence of ascites or when ruptured.
- Associated malformation commonly seen.
- Usually first diagnosable in the second trimester but can be detected in the first trimester if the liver is present within the mass, especially using three-dimensional ultrasound. In physiologic omphalocele, only the gut will be seen in the herniated sac.
- An anterior abdominal wall mass >7 mm at any crown-rump length (CRL), or of any size in a fetus of CRL >44 mm, is suggestive of a fetal anomaly. Alternatively, a cord base mass within the 4-7 mm range for a CRL of 19-44 mm can be considered normal and not to require any follow-up.
- Three-dimensional ultrasound can be useful for additional information and more efficient counseling and postnatal therapeutic planning.
- A false-positive diagnosis of omphalocele, or pseudo-omphalocele, can be produced by scanning in an oblique plane or by compressing the fetal abdomen.
- Main differential diagnoses include:
- Gastroschisis: no surrounding membrane, normal cord insertion
- Umbilical hernia: covered by skin rather than a membrane, indistinguishable from a small omphalocele
- Bladder/cloacal exstrophy: a mass below the cord insertion site with no visible bladder
- Limb-body wall complex: the placenta attached to the fetus, absent or very shortened cord, limbs and spine defects
- Pentalogy of Cantrell: ectopia cordis with omphalocele
- Urachal and omphalomesenteric cyst: cysts at the cord insertion site, no visceral contents
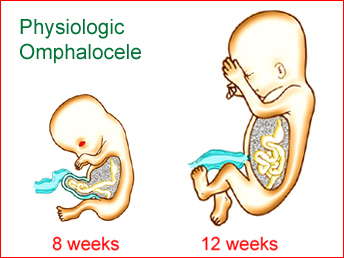
Fig 1: Schematic drawing of physiologic omphalocele at 8 weeks of gestation with the disappearance at 12 weeks
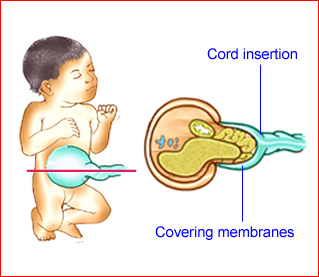
Fig 2: Schematic drawing of omphalocele containing liver and bowel; note the cord insertion on the covering membranes
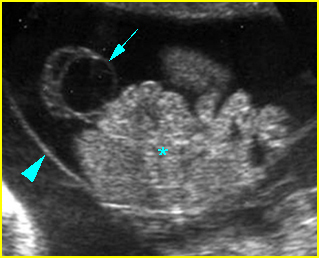
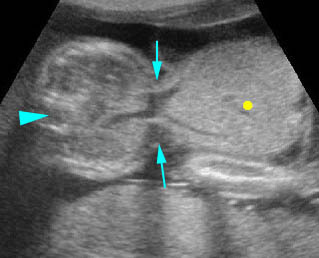
Fig 3: Omphalocele Free floating sac (arrow) containing liver and bowel (*) with covering membrane (arrowhead) (arrow = omentum)
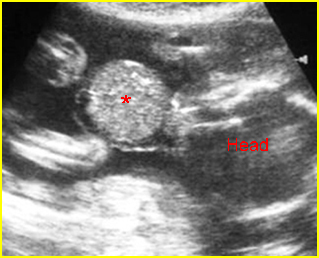
Fig 4: Omphalocele Free floating liver mass with covering membrane (*) in amniotic fluid
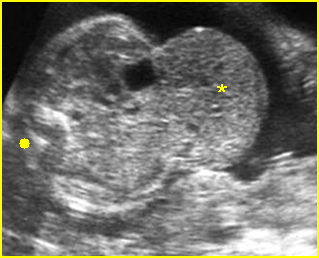
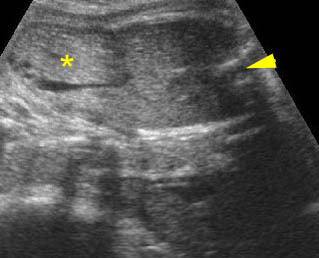
Fig 5: Omphalocele Cross-sectional scan of the abdomen: liver mass (*) protruding through large defect, invisible covering membrane blending with the liver (solid circle = spine)
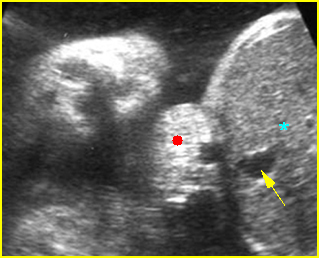
Fig 6: Small omphalocele Cross-sectional scan of the abdomen: small part of the liver (solid circle) protruding through the umbilicus, (* = liver, arrow = umbilical vein)
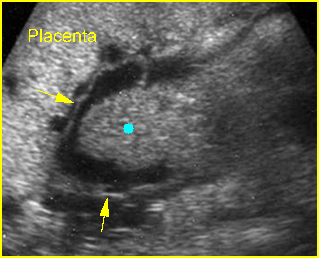
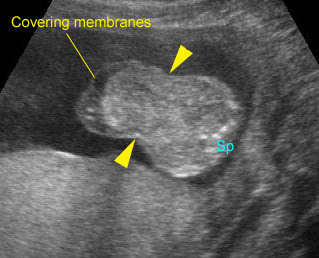
Fig 7: Omphalocele Liver mass (solid circle) with covering membrane (arrows) located outside of the body
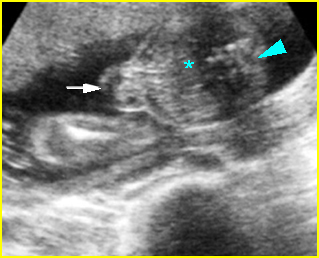
Fig 8: Small omphalocele Cross-sectional scan of the abdomen: bowel (arrow) protruding through the umbilicus (* = liver, arrowhead = spine)
Video clips of omphalocele
Omphalocele: Cross-sectional scan: large omphalocele with liver content (solid circle) (arrow = the defect, arrowhead = spine)
Omphalocele: Liver with covering membranes protruded through the large abdominal wall defect (arrowhead)
Pseudo-omphalocele : The abdomen with liver content (*) protruding anteriorly with intact abdominal wall (arrowhead = spine)
Omphalocele in late first trimester : Liver as well as bowel protruded through the defect at the cord insertion
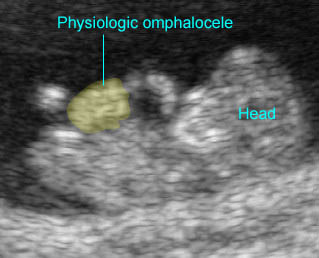
Physiologic omphalocele: Bowel herniated into the proximal cord during 10 weeks of gestation
Associations: Mostly sporadic but associated with other anomalies in 50-85% of cases (cardiac defect in 45-50%, and other anomalies such as neural tube defects, diaphragmatic hernia, etc.), and chromosomal abnormalities in 30% of cases, especially trisomy 18 and 13, particularly when the sac contains no liver and is associated with another anomaly.
Management: A careful search for associated anomalies and karyotyping are indicated. For isolated omphalocele, delivery should occur in a tertiary center with appropriate facilities for surgical management of the newborn. A multidisciplinary approach to the fetus can improve the neonatal outcome. There is still a relatively high rate of elective termination of pregnancies for both defects, even in isolated cases which generally have a good prognosis after surgical repair. Cesarean section probably does not improve the outcomes.
Prognosis: Good for isolated lesions with proper management but poor when associated with other anomalies or chromosome abnormalities.
Recurrence risk: Sporadic for isolated cases, but there is probably a high recurrent rate in cases with rare autosomal dominant or X-linked recessive inheritance.

