Nuchal Translucency (NT)
In the first trimester, the nuchal translucency (NT), instead of the nuchal fold, is used due to its sonographic appearance. NT normally increases with gestation and crown-rump length. It increases with crown-rump length and the median NT increases from 1.2 mm at 11 weeks to 1.9 mm at 13+6 weeks. Thickened NT may be due to fetal cardiac failure, abnormalities of the extracellular matrix, or abnormalities of the lymphatic system.
During the second trimester, NT usually resolves and in a few cases it evolves into either nuchal edema or cystic hygromas with or without hydropic changes. Extensive studies have now established that fetal NT, using the value of the 95th percentile for crown-rump length as a cut-off point, can effectively screen Down’s syndrome with a sensitivity of at least 75% for a false positive rate of <5%. In addition, the thickened NT is also associated with numerous syndromes (e.g. Cornelia de Lange, Noonan syndrome, Smith-Lemli-Opitz syndrome, Apert syndrome) or anomalies in euploid fetuses (e.g. major heart defects, diaphragmatic hernia) , and adverse outcome (early fetal demise) .
Sonographic measurement:
NT can be measured successfully by transabdominal ultrasound in about 95% of cases; in the other cases, it is necessary to perform transvaginal sonography. The average time allocated for each fetal scan should be at least 10 minutes. All sonographers performing fetal scans should be capable of reliably measuring the crown-rump length and obtaining a proper sagittal view of the fetal spine. It is essential that the same criteria are used to achieve uniformity of results among different operators:
- The minimum fetal crown-rump length should be 45 mm and the maximum 84 mm. The optimal gestational age for measurement of fetal nuchal translucency is 11-13+6 weeks.
- The results from transabdominal and transvaginal scanning are similar but the reproducibility may be better with the transvaginal method.
- A good sagittal section of the fetus, as for measurement of crown-rump length, should be obtained.
- The magnification should be such that the fetus occupies at least three-quarters of the image. Essentially, the magnification should be increased so that the increment in the distance between the calipers should be only 0.1 mm.
- Care must be taken to distinguish between fetal skin and amnion because, at this gestation, both structures appear as thin membranes. This is achieved by waiting for spontaneous fetal movement away from the amniotic membrane; alternatively, the fetus is bounced off the amnion by asking the mother to cough and/or by tapping the maternal abdomen.
- The maximum thickness of the subcutaneous translucency between the skin and the soft tissue overlying the cervical spine should be measured by placing the calipers on the lines as shown in Fig.<?which figure?>. During the scan, more than one measurement must be taken and the maximum one should be recorded.
- The NT should be measured with the fetus in the neutral position. When the fetal neck is hyperextend the measurement can be increased by 0.6 mm and when the neck is flexed the measurement can be decreased by 0.4 mm.
- The umbilical cord may be around the fetal neck in 5-10% of cases and this finding may produce a falsely increased nuchal translucency, adding about 0.8 mm to the measurement. In such cases, the measurements of NT above and below the cord are different and, in the calculation of risk, it is more appropriate to use the smaller measurement.
The ability to measure NT and obtain reproducible results improves with training; good results are achieved after 80 and 100 scans for the transabdominal and the transvaginal routes, respectively. Appropriate training, high motivation and adherence to a standard technique for the measurement of NT are essential prerequisites for good clinical practice.
In two large multicenter studies of first trimester Down’s syndrome screening, accurate nuchal translucency measurements required stringent training, formalized evaluation of sonographers’ competence, and continuing external quality control. In the latter trial, adequate NT images could not be obtained in 6% of cases.
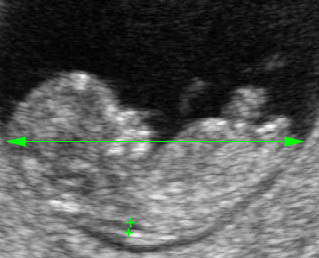
Nuchal translucency: Mid-sagittal scan of the fetus at 11 weeks of gestation showing NT and crown-rump length measurements
Thickened nuchal translucency: Mid-sagittal scan of the fetus at 11 weeks of gestation showing the NT of 3.0 mm
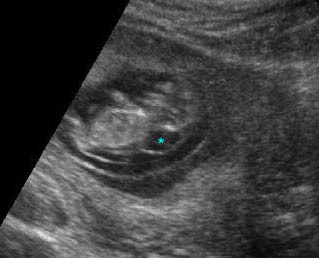
Thickened nuchal translucency : Sagittal scan of the fetus 10 weeks: cystic lesion (*) on the fetal neck
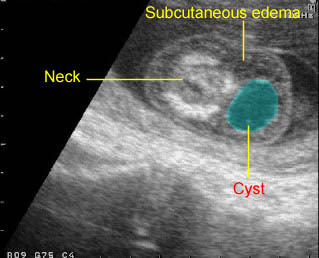
Early cystic hygroma : Small non-septate cyst on the back of the neck with early hydrops fetalis (subcutaneous edema)
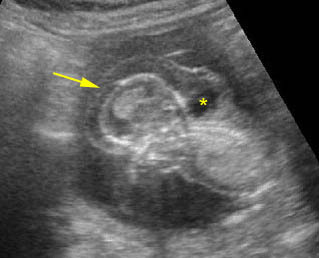
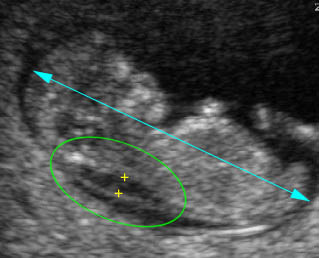
Early hydrops fetalis: Sagittal scan of the fetus 13 weeks: generalized subcutaneous edema (arrow) with cystic fluid collection (on the back of the neck) (hydrops fetalis related to cystic hygroma)
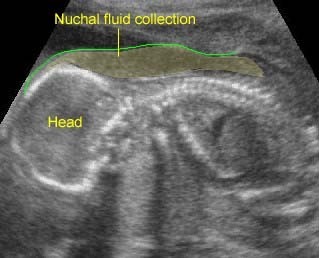
Markedly Thickened NT: Nuchal fluid collection at the posterior aspect of the neck of the fetus with monosomy X

