Cleft Lip/Palate
Natural history: multifactorial (more than 90%), part of several syndromes or chromosome abnormalities in <10%, most are trisomy 18 and 13.
Clefts are classified into five categories:
- Type 1, cleft lip alone; a lower rate of anomalies (20%)
- Type 2, unilateral cleft lip and palate; intermediate prognosis
- Type 3, bilateral cleft lip and palate; intermediate prognosis
- Type 4, midline cleft lip and palate; a high rate of concurrent anomaly, fatal outcome
- Type 5, slash type; facial defects associated with amniotic bands or limb-body wall complex; a high rate of concurrent anomaly, fatal outcome.
Incidence: 1 in 1000 live births but much more common among prenatal series.
- Isolated lesion accounting for about two-thirds of clefts and about one-third have associated abnormalities.
- Isolated cleft lip and/or palate in 0.8 per 1000 births (cleft lip alone 0.3, cleft lip and palate 0.5 per 1000). There is marked ethnic and racial variation. Non-Hispanic Whites had the greatest prevalence of isolated clefts, Asians had a slightly lower prevalence, and Blacks had the lowest prevalence.
- Isolated cleft palate (distinct disorder); 0.31 per 1000 births. Asians had the lowest prevalence of CP; in Whites and Hispanics it was almost twice as high.
Sonographic findings:
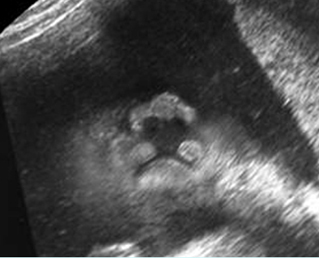
Fig 1, Fig 2, Fig 3, Fig 4
- Defect of the upper lip which is most easily detected in the coronal view.
- Cleft palate best diagnosed by showing disruption of the C-shaped alveolar ridge of the maxilla in the axial view.
- In the presence of a bilateral cleft lip/palate a mass of soft tissue (premaxillary protrusion) protrudes anteriorly residing beneath the nose.
- A maxillary protrusion best visualized in the sagittal plane.
- Most fetuses with bilateral cleft lip and palate often show a protuberant premaxillary segment, a midline echogenic soft tissue mass just below the nose, whereas some have no premaxillary segment but show a flattened nose instead.
- Midline clefts: an absence of the central maxilla and upper lip with a deformed or small or absent nose, commonly associated with proboscis.
- Slash types: asymmetric random defects caused by amniotic bands.
- 3D ultrasound or MRI may be ancillary to conventional ultrasound in prenatal diagnosis of the facial cleft, allowing a better staging of the lesion by demonstrating the degree of involvement of the palate.
- Pitfalls:
- For isolated clefts, the detection rate for isolated lesions varies among studies from 18 to 75%.
- Normal philtrum can sometimes be confused with a midline cleft lip.
- Premaxillary protrusion associated with bilateral cleft can be confused with other facial masses.
- Bilateral clefts without premaxillary segment are likely to be confused with large midline cleft.

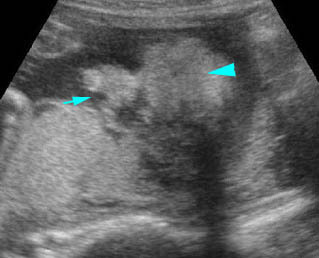
Median cleft lip Coronal view of the face: median cleft lip in fetal trisomy 13
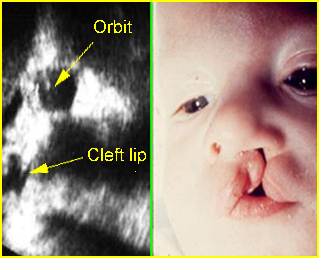
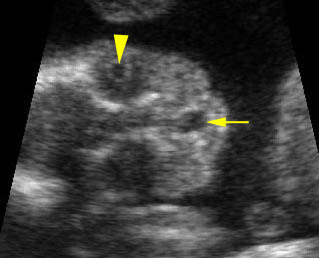
Paramedian cleft Sagittal view of the face: paramedian cleft lip
Median cleft lip Coronal view of the face: median cleft lip in fetal trisomy 13
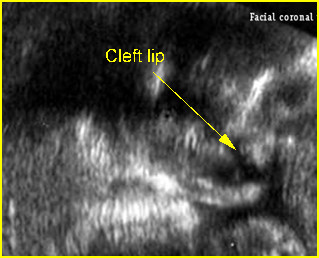
Paramedian cleft Coronal view of the face: paramedian cleft lip (arrow)
Video clips of cleft lip / palate
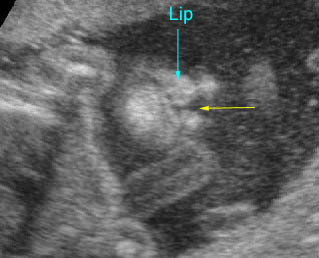
Cleft lip: Coronal scan of the face: small paramedial cleft (arrow)
Cleft lip: Coronal scan of the face: paramedial cleft (arrow)

Bilateral cleft lips : Coronal scan of the face: bilateral paramedial cleft (arrow)

Cleft lip and palate : Transverse scan of the face: incomplete alveolar ridge (*) of the maxilla
Midline cleft lip: Coronal scan of the face: midline cleft (arrow) (arrowhead = lens in the orbit)
Associations: One-third of the fetuses with clefts are associated with other anomalies, including more than 250 syndromes, especially central nervous system and cardiac anomalies. Chromosomal abnormalities are seen in about 10%, especially trisomy 18 and 13. Midline clefts, accounting for <1% of all facial clefts, are commonly related to holoprosencephaly and trisomy 13.
Management: Careful prenatal and postnatal search for associated anomalies is required. All continuing pregnancies should be karyotyped. Serial sonography should be performed. Antenatal diagnosis and antenatal counseling are very important for either planned postnatal therapy or termination in cases with fatal anomalies.
Prognosis: Good unless other severe anomalies are present. Poor prognosis when related to other anomalies and chromosomal abnormalities.
Recurrence risk: For isolated cases, 4% of recurrent risk with one affected sibling, 9% with two affected siblings, 4% with one affected parent and 17% with one affected sibling and one affected parent. Folic acid supplementation may decrease the risk of recurrence.

