Osteogenesis Imperfecta (OI)
Osteogenesis Imperfecta (OI)
OI is genetically a heterogeneous disorder consisting of both autosomal dominant and autosomal recessive entities caused by mutations in one or two structural genes for type I procollagen. The clinical heterogeneity is due to the different mutations in the genes: COL1A1 and COL1A2. OI is divided into four types as follows:
- Type I (autosomal dominant) is characterized by bone fragility, blue sclera, hearing loss, and normal calvarium, with fractures ranging from none to multiple. DNA-based analysis is possible for early prenatal diagnosis.
- Type II (new dominant mutations and autosomal recessive in <5%) is a perinatal lethal variety characterized by almost no ossification of the skull, beaded ribs, shortened crumpled long bones and multiple fractures in utero.
- Type III (autosomal recessive, rare) is a non-lethal variety characterized by blue sclera (becoming white with time) and multiple fractures present at birth.
- Type IV (autosomal dominant) is the mildest form (mild to moderate osseous fragility). Long bones and sclera are normal.
Incidence: 0.4 per 10,000 births for OI, and 0.2 per 10,000 births for OI type II.
Sonographic findings (OI type II) :
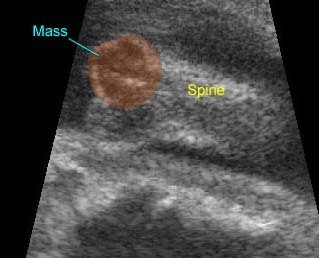
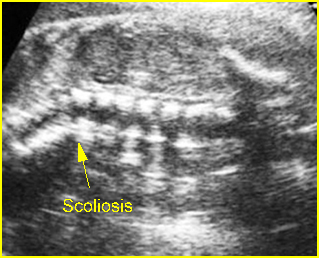
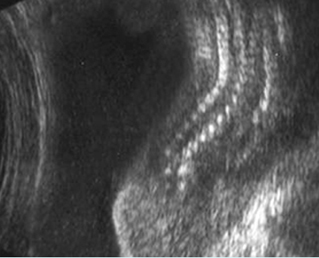
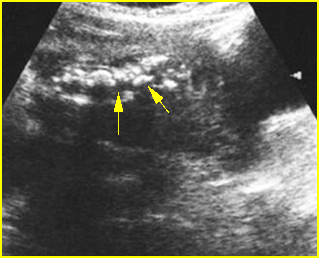
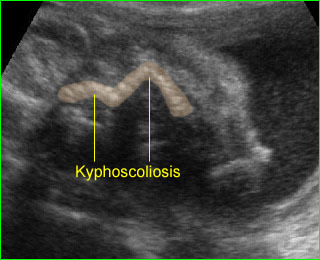
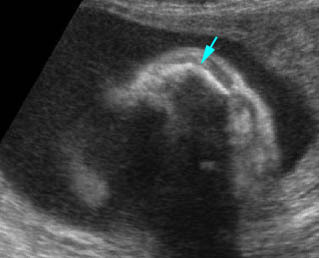
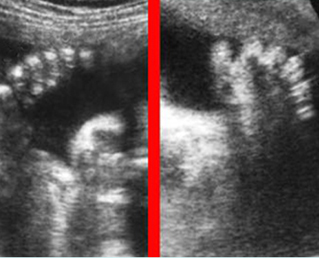
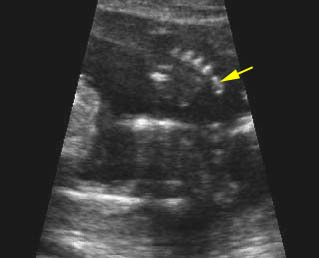
Fig 1, Fig 2, Fig 3, Fig 4, Fig 5, Fig 6
- Variable hypomineralization, which may result in complete absence of acoustic shadow and may be so severe that the normally-difficult-to-visualize near-field brain is easily seen.
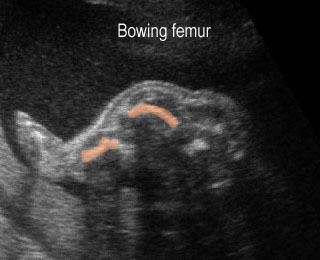
- Micromelia (type IIB and IIC may be less severe).
- Fractures of long bones.
- Thickened long bones due to frequent fractures and secondary callus formation.
- Small bell-shaped thorax with multiple rib fractures or beaded ribs.
- Increased nuchal translucency thickness in the first trimester in some cases.
- MRI complemented sonography may be helpful in further differentiating clinical and sonographic findings.
- Sonographic features are variable among the three subtype as follows:
- Type IIA: thick bones, multiple fractures, hypomineralization, beaded ribs
- Type IIB: thick bones, multiple fractures, less beading of ribs; lower extremities are affected more than upper extremities
- Type IIC: thin bones, multiple fractures, thin beaded ribs.
- Pitfalls: Variable short limb lengths without fractures may be the only clue in the mild form.
- Usually diagnosed in the second and third trimesters but possible in the late first trimester.
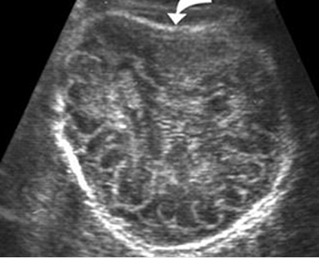
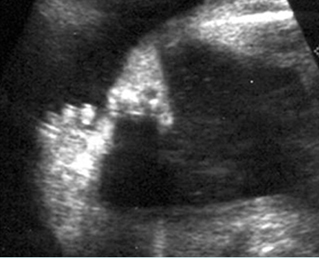
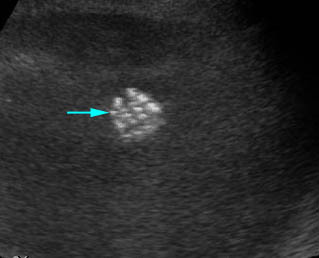
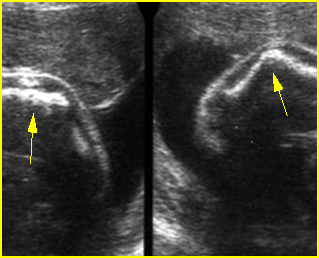
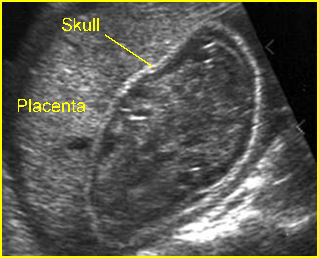
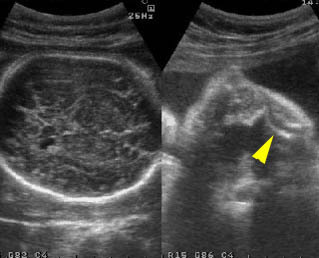
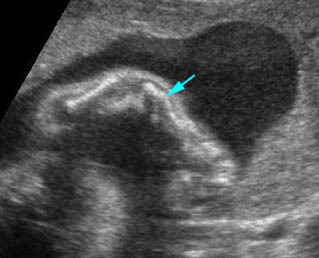
Fig 1: Sonolucent and compressible skull Poorly ossified and compressible cranium (arrow), cerebral sulci and gyri could easily be seen

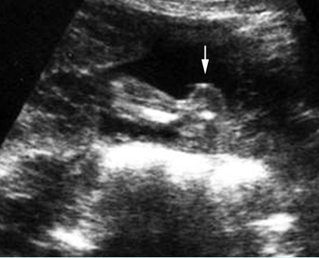
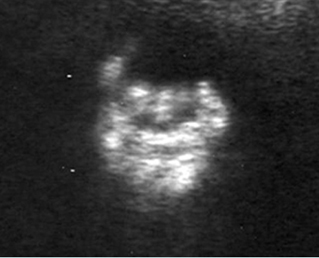
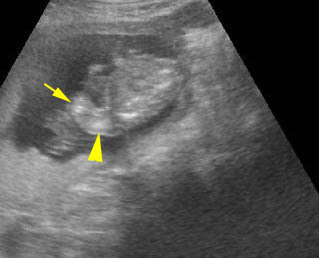
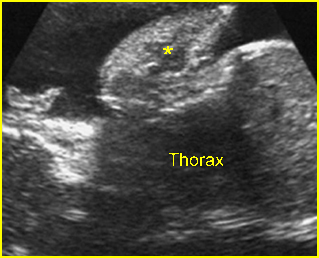
Fig 2: Rib fractures Multiple rib fractures with poor ossification in the fetus with osteogenesis imperfecta type IIA
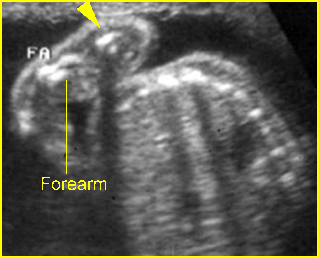
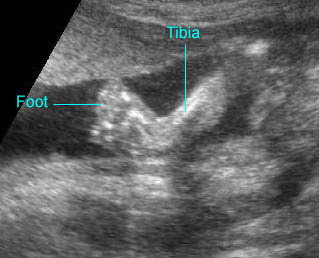
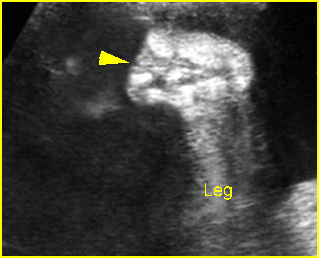
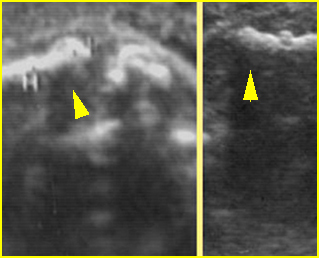
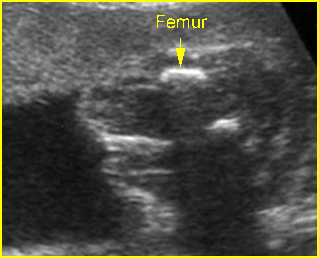
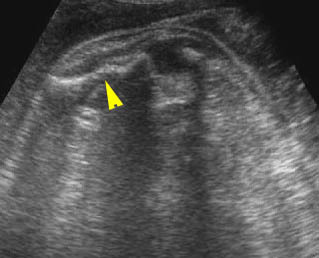
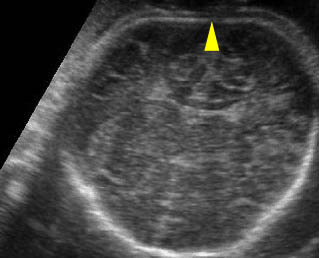
Fig 3: Micromelia Irregularity and severe shortening of long bone (arrowhead)
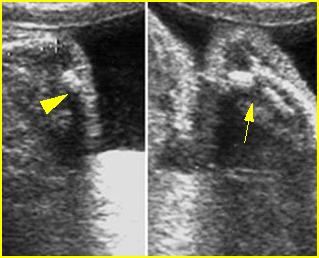
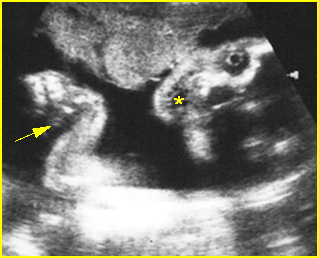
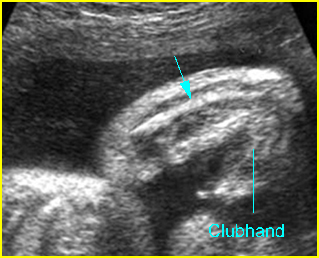
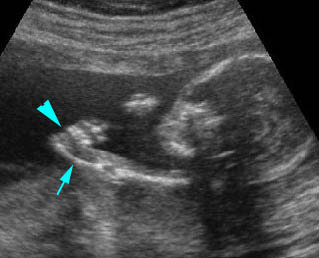
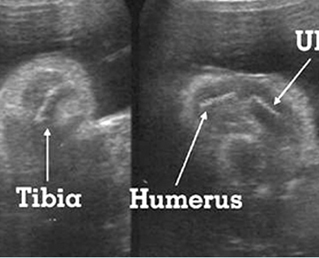
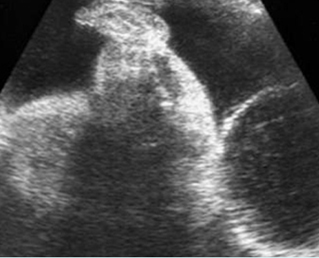
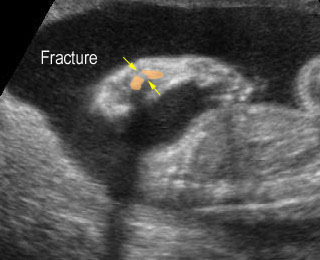
Fig 4: Fracture in utero Longitudinal scan of upper extremity: poorly ossified and fracture in osteogenesis imperfecta type IIA
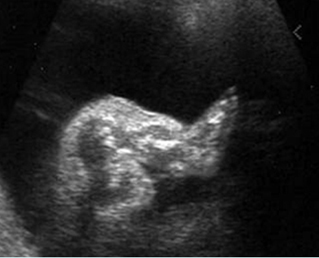
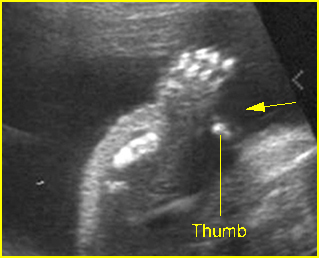
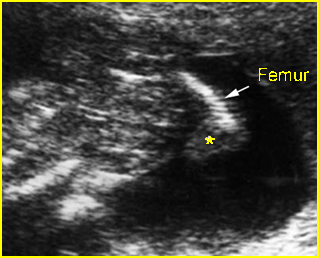
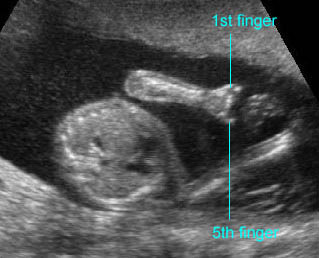
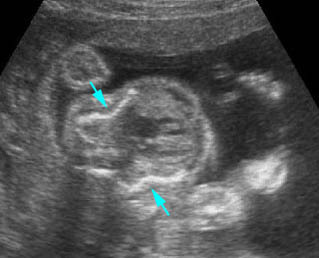
Fig 5: Osteogenesis imperfecta type IIA Longitudinal scan of lower extremity: shortened and irregular ossified long bones
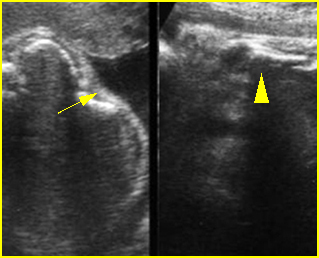
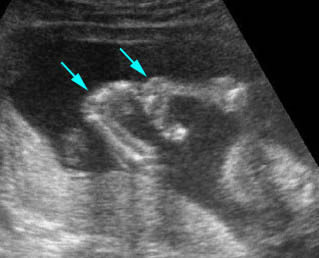
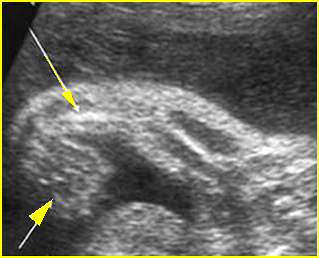
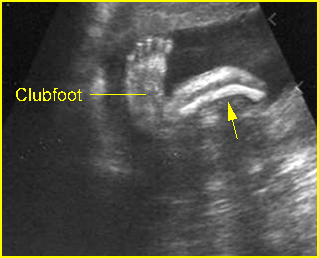
Fig 6: Fracture of long bones Longitudinal scan of rib and humerus: fracture rib (arrow) and humerus (arrowhead) with moderate ossification
Video clips of osteogenesis imperfecta (OI)
Osteogenesis imperfecta (IIA) : Irregular long bone (arrowhead) with poorly ossified
Osteogenesis imperfecta (IIA) : Cross-sectional scan of the thorax: rib fractures (arrow)
Osteogenesis imperfecta: Long bone fracture of the forearm
Fracture in utero : Longitudinal scan of upper limb: callus formation (arrow) and irregularity of ulna secondary to previous fracture
Sonolucent skull : The thin skull is so poorly ossified that cerebral gyri and sulci could be seen easily
Associations: Rare, though concurrent anencephaly has been reported.
Management: Termination of pregnancy can be offered. For term pregnancy, cesarean delivery does not decrease fracture rates at birth in infants with non-lethal forms of OI.
Prognosis: OI type II is lethal.
Recurrence risk: Unlikely because OI type II is due to new mutations in most cases and there are only a few reports of autosomal recessive inheritance.