Sacral Agenesis
The spectrum of sacral agenesis and dysgenesis is associated with caudal regression syndrome (CRS) and sirenomelia (mermaid syndrome). Considerable overlap between these abnormalities may exist, with some considering them spectrums of the same entity. A more recent theory, however, suggests that CRS and sirenomelia are pathologically distinct entities.
Caudal Regression Syndrome (CRS)
CRS refers to abnormalities associated with the absence of the sacrum and variable portions of the lumbar spine. This malformative syndrome is mainly seen in cases of maternal diabetes with poor metabolic control.
Incidence: Rare, with an increased frequency in infants of diabetic mothers (200 times, but <1%), or with retinoic exposure in utero.
Sonographic findings:
- Absence of sacrum and variable portions of the lumbar or even thoracic spine.
- Abrupt interruption of the spine at the dorsal or lumbar level.
- Abnormal position of the lower limbs.
- Abnormal pelvic bone, e.g. small, apposed, or absent.
- The femur bones are of fixed flexion and abduction in a Buddha position.
- A two-vessel umbilical cord may be seen but this is not as common as with sirenomelia.
- Increased frequency of renal abnormalities, e.g. agenesis, cystic dysplasia.
- Oligohydramnios in cases of renal agenesis.
- Polyhydramnios is occasionally seen if the patient is diabetic.
- Increased nuchal translucency in late first trimester.
- Diagnosable in late first trimester, especially with transvaginal ultrasound.
- The sequence of development of the sacral region ossification is related to gestational age. When the S1-S2 ossification nuclei are visualized at 16-17 weeks of gestation, isolated sacral agenesis can be accurately excluded.
Associations: Non-specific anomalies involving any system may be found.
Management: Termination of pregnancy should be offered. In continuing pregnancy, a multidisciplinary approach is required.
Prognosis: Poor, but in some selected cases a better outcome may be achieved with multidisciplinary management.
Recurrence risk: Rare, however with maternal diabetes or familial history the recurrence risk is higher.
Sirenomelia
Sirenomelia or mermaid syndrome refers to a complex malformation caused by disruptive vascular defects, characterized by a single lower extremity, associated with renal agenesis, and absence of the sacrum. Sirenomelia may be due to an alteration in early vascular development leading to vitelline arterial steal, in which the blood flow is diverted from the caudal region of the embryo to the placenta, resulting in multiple defects of the lower extremities. A single lower extremity in sirenomelia arises from failure of the lower limb bud field to be cleaved into two lateral masses.
Incidence: 1 in 24,000-67,000 births.
Sonographic findings:
- Fusion of the lower extremities, the flipper-like deformity of the foot.
- Lower spine deformities.
- Bilateral renal agenesis, leading to oligohydramnios.
- The fibulas, if present, are between the tibia.
- The sole of the foot is oriented ventrally instead of dorsally.
- Single umbilical artery.
- Situs inversus is frequently seen.
- Three-dimensional ultrasound is helpful in the diagnosis.
- Diagnosable in late first trimester, especially with transvaginal ultrasound.
- The main differential diagnosis is caudal regression syndrome.
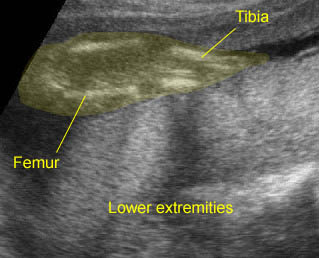
Sirenomelia : Fusion of the both lower extremities; the both extrremities persistently close to each other
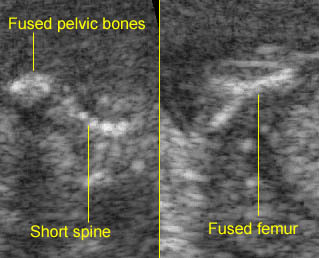
Sirenomelia : Short spine with fused pelvic bones and Y-shaped fused femur
Associations: Non-specific anomalies involving any system may be found.
Management: Termination of pregnancy should be offered.
Prognosis: Lethal, though an infant with sirenomelia surviving beyond the neonatal period was reported (now 4 years old).
Recurrence risk: Rare, however with maternal diabetes or familial history the recurrence risk is higher.

