Fetal Cardiac Examination
Congenital heart disease (CHD) is a leading cause of infant mortality with an estimated incidence of 4-8 per 1000 live births. Nonetheless, structural cardiac defects are among the most frequently missed abnormalities by prenatal ultrasound. Although currently prenatally diagnosed CHD is substantially improved, most cases world-wide are not prenatally diagnosed. The screening four-chamber view (FCV) may detect only 50-60% of cardiac anomalies and additional views of the outflow tracts will increase the sensitivity to 75%. The American Institute of Ultrasound in Medicine (AIUM) have introduced guidelines for cardiac screening, including examination of the four-chamber view and also outflow tracts. Furthermore, the level of operator experience is also an important factor that should be considered for fetal cardiac screening. Generally, fetal echocardiography is an extremely useful and accurate clinical tool for evaluation of a congenital heart with concordance of prenatal and postnatal echocardiography. When an abnormality is suspected, full fetal echocardiography should be performed. The scope of cardiac examination includes
- basic cardiac examination: focus on the four-chamber view; this is the minimal requirement for standard examination
- extended cardiac examination: including the outflow tracts; if technically feasible, this should be done on standard examination
- full fetal echocardiography: complete cardiac examination which should be done as a specialized examination in suspected cases of CHD or pregnancies at risk, for example; intracardiac echogenic foci which increases the risk of Down’s syndrome five- to seven-fold.
Fig 1, Fig 2, Fig 3, Fig 4, Fig 5, Fig 6, Fig 7, Fig 8
Basic Cardiac Examination (FCV)
Fig 9, Fig 10, Fig 11, Fig 12
General considerations:
- The examination can be performed optimally between 18 and 22 weeks of gestation.
- Cardiac structures are often well visualized when the left ventricular apex is directed anteriorly toward the maternal abdominal wall, although there may be limitations secondary to improper fetal position, maternal obesity, and abdominal scar.
- Chamber disproportion can sometimes be better appreciated when the interventricular and interatrial septae are perpendicular to the ultrasound beam.
- Higher frequency transducers will improve the likelihood of detecting subtle defects but at the expense of reduced penetration.
- A normal cardiac rate and regular rhythm should be confirmed. Heart rate typically ranges from 120 to 160 bpm.
- The heart axis is normally deviated about 45+20 (2 SD) degrees toward the left side of the fetus. An abnormal axis increases the risk of a cardiac malformation.
- A normal small hypoechoic rim around the fetal heart can be mistaken for a pericardial effusion.
- The basic screening examination entails a critical analysis of the FCV and outflow tracts. Correct analysis of the four-chamber view and both outflow tracts will exclude the majority of cases of serious congenital heart disease.
Technique: FCV
After determining the heart location within the left side of the chest, the same size<?should this be “side”? see below> as the stomach, the fetal thoracic spine is identified and then FCV is obtained from an axial plane across the fetal thorax. Anatomically, the right ventricle is behind the sternum, and the left ventricle is inferior and to the left of the right ventricle.
Checklist for Fetal Cardiac Screening Examination
General
- Four cardiac chambers are present
- The majority of the heart is located in the left chest, on the same size<?should this be “side”? see above> as the stomach
- The heart occupies about one-third of the thoracic area
- Normal cardiac situs, axis, and position
- Heart beats regularly within normal limits for the fetal rate
- No fluid accumulation is seen (pericardium, and pleural space)
Atria
- Atria appear approximately equal in size
- The foramen ovale flap moves within the left atrial chamber
- The ostium primum attaches to the interventricular septum
- The lower rim of atrial septum (septum primum) is present
- Caval veins drain into the right atrium
- Visualization of the pulmonary veins with B-mode ultrasound aided by color-flow Doppler can be accomplished in the majority of fetuses, while the four-chamber view is studied
Ventricles
- Ventricles approximately equal in size, shape and wall thickness, without hypertrophy
- Moderator band present at the right ventricular apex
- Ventricular septum appears completely intact from apex to crux
AV Valves
- Both atrioventricular valves are open and move freely
- The septal insertion of the tricuspid valve is slightly lower than the mitral valve (normal off-setting of the atrioventricular valves).
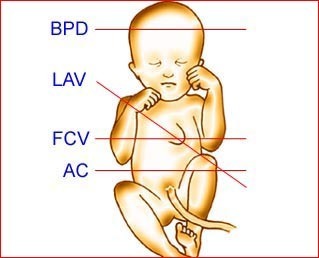
Fig 1: Schematic drawing: The planes for four-chamber view (FCV) and long axis view (LAV) of the heart (BPD = biparietal diameter, AC = abdominal circumference)
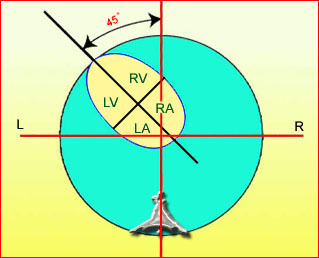
Fig 2: Schematic drawing: Four-chamber view with typical cardiac axis, normal size and appropriate location (LA = left atrium, LV = left ventricle, RA = right atrium, RV = right ventricle)
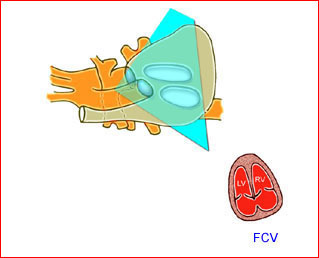
Fig 3: Schematic drawing : The plane of the four-chamber view obtained from an axial scanning plane across the fetal thorax
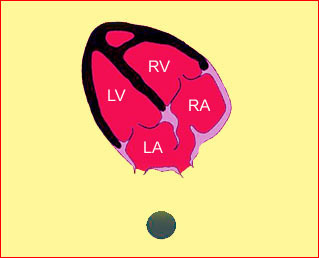
Fig 4: Schematic drawing: Four-chamber view in relation to fetal spine; left atrium (LA) close to the spine and moderator band noted in the right ventricle (RV) (RA = right atrium, LV = left ventricle)
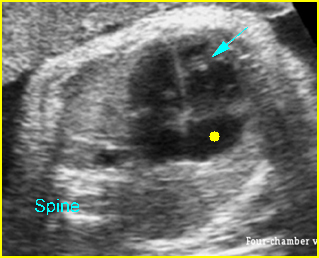
Fig 5: Normal four-chamber view Cross-sectional scan of thorax: normal four-chamber view (arrow = moderator band in right ventricle, solid circle = right atrium)
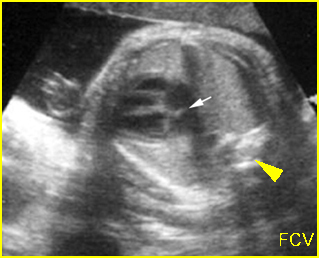
Fig 6: Foramen ovale Four-chamber view: normal four chambers (arrow = foramen ovale, arrowhead = spine)
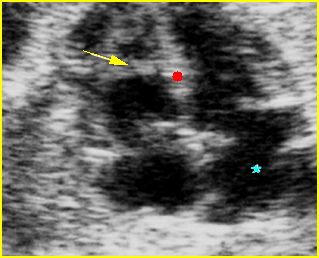
Fig 7: Moderator band Four-chamber view: normal four chambers, moderator band (arrow) in the right ventricle (* = left atrium)
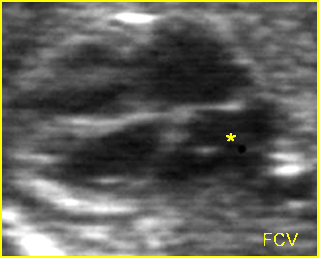
Fig 8: Normal four-chamber view Four-chamber view: normal four chambers, * = left atrium
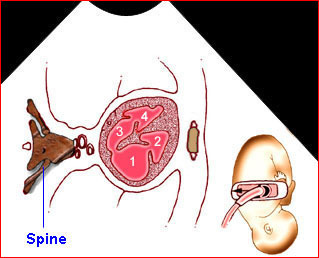
Fig 9: Schematic drawing: Four-chamber view in relation to fetal position (1 = right atrium, 2 = right ventricle, 3 = left atrium, 4 = left ventricle)
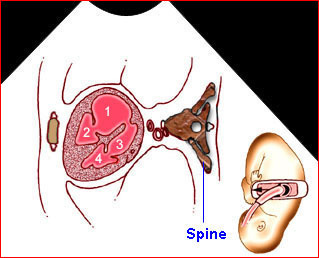
Fig 10: Schematic drawing: Four-chamber view in relation to fetal position (1 = right atrium, 2 = right ventricle, 3 = left atrium, 4 = left ventricle)
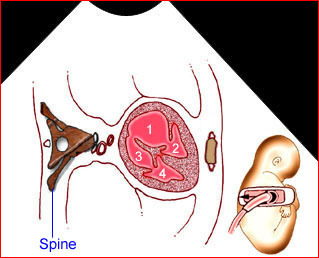
Fig 11: Schematic drawing: Four-chamber view in relation to fetal position (1 = right atrium, 2 = right ventricle, 3 = left atrium, 4 = left ventricle)
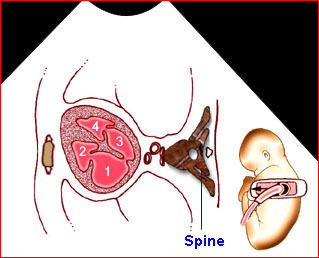
Fig 12: Schematic drawing: Four-chamber view in relation to fetal position (1 = right atrium, 2 = right ventricle, 3 = left atrium, 4 = left ventricle)
Video clips of the normal heart
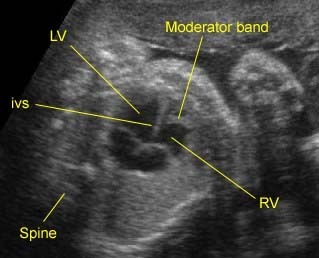
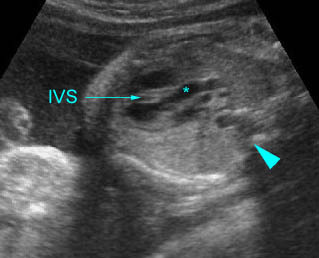
Normal four-chamber view: Typical four-chamber view: note the moderator band in the right ventricle (RV) (LV = left ventricle, IVS = interventricu-lar septum)
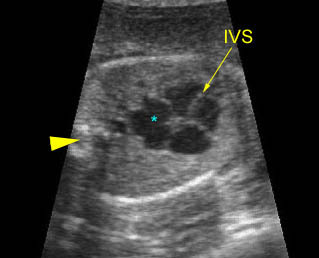
Normal four-chamber view: Four-chamber view: * = left atrium, arrowhead = spine
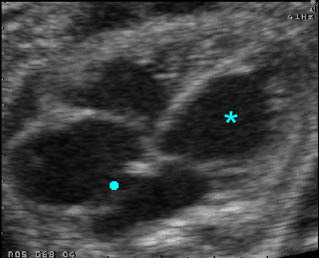
Four-chamber view: Solid circle = foramen ovale, * = left ventricle, note the relationship between tricuspid and mitral valve insertion
Extended Basic Examination
If technically feasible, optional views of the outflow tracts can be obtained as part of an extended cardiac screening examination. Evaluation of outflow tracts can increase the detection rates for major cardiac malformations above that achievable by the FCV alone. This exam minimally requires that normal great vessels are approximately equal in size and that they cross each other at right angles from their origins as they exit from their respective ventricular chambers. Failure to confirm these criteria in a well-visualized study should alert the examiner that a more detailed evaluation may be warranted.
Fig 13, Fig 14, Fig 15, Fig 16, Fig 17, Fig 18, Fig 19
Technique: Outflow tract
The outflow tracts are typically obtained by angling the transducer toward the fetal head from a FCV when the interventricular septum is tangential to the ultrasound beam. A supplementary technique for evaluating the outflow tracts has also been described for the fetus when the interventricular septum is perpendicular to the ultrasound beam.
Left Ventricular Outflow Tract (LVOT)
Fig 20, Fig 21
The relation of the aortic root and left ventricle is best evaluated by the left ventricular long-axis view. This view is obtained by rotating the transducer from the FCV into a plane angled from the fetal stomach toward the right shoulder of the fetus. This plane is easiest obtained when the interventricular septum is perpendicular to the ultrasound beam in the FCV. This view may detect small ventricular septal defects and conotruncal abnormalities that are not seen on FCV. This view confirms the presence of a great vessel originating from the left ventricle. Continuity should be documented between the anterior aortic wall and ventricular septum. The aortic valve should be freely moving and not thickened.
When the LVOT is definitely the aorta, it may even be possible to trace the vessel into the arch from which three arteries originate into the neck.
Right Ventricular Outflow Tract (RVOT)
Fig 22, Fig 23
After examining the left ventricle and aortic outflow tract, tilt the transducer towards the anterior chest wall until the right outflow tract is imaged, which is perpendicular to the LVOT. Once this is accomplished, the main pulmonary artery is identified as it exits the right ventricle. It is slightly larger than the aortic root. The RVOT normally exits the right ventricle perpendicular to the more posteriorly positioned ascending aorta. The pulmonary outflow valve should be freely moving and not thickened. The RVOT can be confirmed as a pulmonary artery only if its distal end appears bifurcated. It divides toward the left side into the ductus arteriosus, which is contiguous with the descending aorta. The right side branches into the right pulmonary artery.
Summary
3 steps for outflow tract examination:
- FCV: Once the FCV is identified, the ultrasound beam is directed perpendicular to the interventricular septum by sliding or rocking the probe at the maternal abdomen.
- LVOT: After adjusting the FCV, the transducer is rotated approximately 45 degrees. In this position, the ultrasound beam is oriented in a diagonal plane from the fetal stomach toward the right shoulder.
- RVOT: After imaging the LVOT, the transducer is kept in the same position and is then rocked, or tilted towards the anterior chest wall of the fetus to image the right outflow tract.
Out flow tract checklist
- The ascending aorta and the main pulmonary artery are perpendicular to each other as they exit their respective ventricles.
- The aortic and pulmonary valves are similar in size.
- The outflow portion of the right ventricle merges with the main pulmonary artery. The pulmonary valve separates these two structures.
- The main pulmonary artery bifurcates into the right and left pulmonary arteries.
- The innominate, left common carotid, and/or the left subclavian arteries should be identified originating from the aortic arch.
- The right pulmonary artery is inferior and perpendicular to the aortic arch.
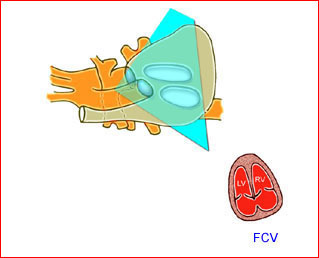
Fig 13: Schematic drawing: The plane of the four-chamber view obtained from an axial scanning plane across the fetal thorax
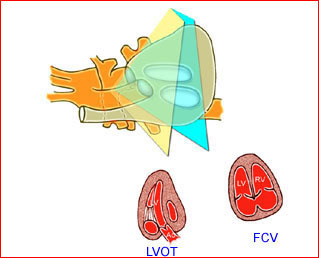
Fig 14: Schematic drawing: Left outflow tract view obtained by angling and slightly rotating the transducer from the four-chamber view toward the fetal head
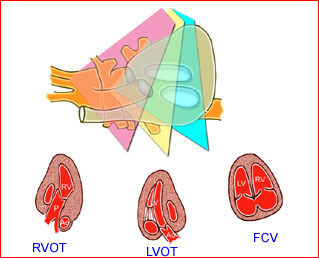
Fig 15: Schematic drawing: Right outflow tract view obtained by angling the transducer from the left outflow tract view toward the fetal head
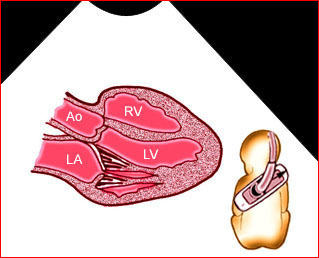
Fig 16: Schematic drawing: Long-axis view in relation to fetal position (Ao = aortic root, LA = left atrium, LV = left ventricle, RV = right ventricle)
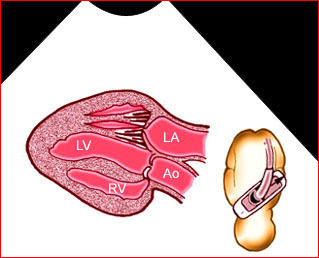
Fig 17: Schematic drawing: Long-axis view in relation to fetal position (Ao = aortic root, LA = left atrium, LV = left ventricle, RV = right ventricle)
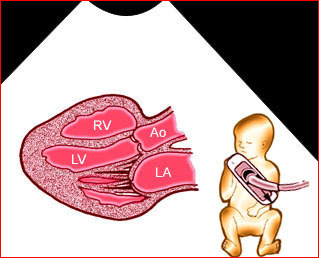
Fig 18: Schematic drawing:Long-axis view in relation to fetal position (Ao = aortic root, LA = left atrium, LV = left ventricle, RV = right ventricle)
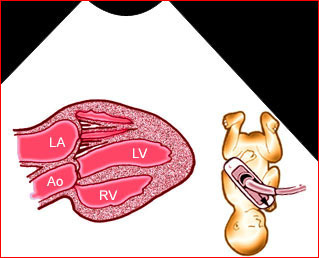
Fig 19: Schematic drawing: Long-axis view in relation to fetal position (Ao = aortic root, LA = left atrium, LV = left ventricle, RV = right ventricle)
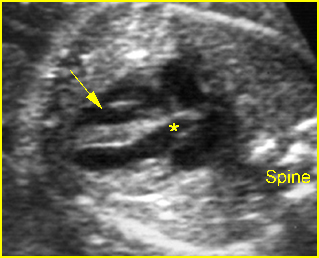
Fig 18: Aortic root Long axis view of the heart: normal aortic root (*) exiting the left ventricle (arrow = right ventricle)
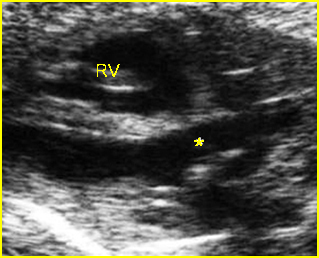
Fig 21: Aortic root Long axis view of the heart: normal aortic root (*) exiting the left ventricle
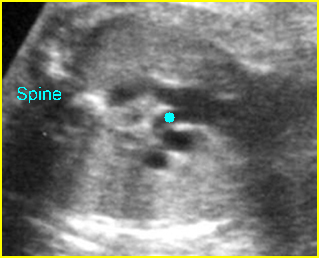
Fig 22: Normal great vessel view Cross-sectional scan at the upper thorax: the relation of superior vena cava, ascending aorta, and pulmonary trunk in order (solid circle = right pulmonary artery arising from pulmonary trunk)
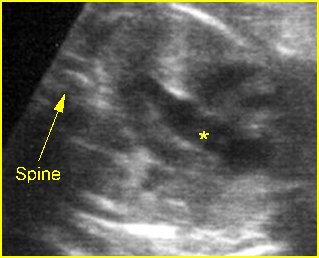
Fig 23: Pulmonary trunk Long axis view of the heart: normal pulmonary root (*) exiting the right ventricle
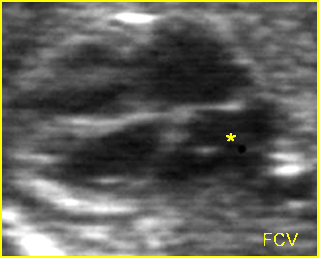
Fig 24: Normal four-chamber view Four-chamber view: normal four chambers, * = left atrium
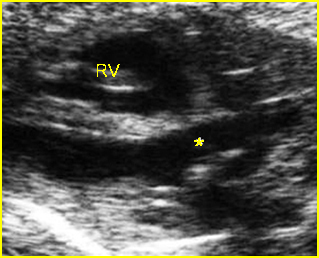
Fig 25: Aortic root Long axis view of the heart: normal aortic root (*) exiting the left ventricle
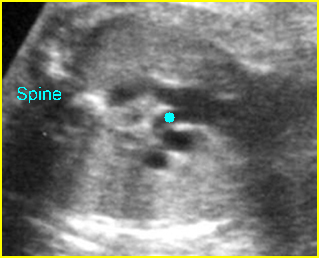
Fig 26: Normal great vessel view Cross-sectional scan at the upper thorax: the relation of superior vena cava, ascending aorta, and pulmonary trunk in order (solid circle = right pulmonary artery arising from pulmonary trunk)

Fig 27: Normal great vessel view Cross-sectional scan at the upper thorax: the relation of superior vena cava (3), ascending aorta (2), and pulmonary trunk (1)
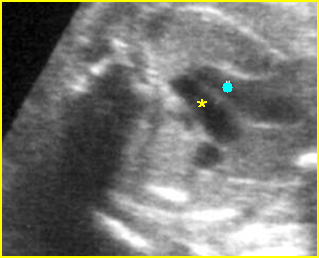
Fig 28: Normal aortic arch Cross-sectional scan of the upper thorax: aortic arch (*) and ductal arch (solid circle) running parallel to the descending aorta
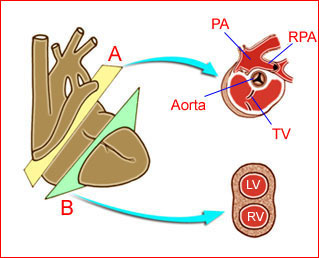
Fig 29: Schematic drawing of the plane for short-axis view (PA = pul-monary trunk, RPA = right pulmonary artery, TV = tricuspid valve, LV = left ventricle, RV = right ventricle)
Video clips of the normal heart
Normal aortic root : Long axis view: * = aortic root, arrowhead = spine
Long-axis view :
1) aortic root arising from left ventricle (solid circle) (* = right ventricle)
2) pulmonary trunk arising from right ventricle, (* = ascending aorta)
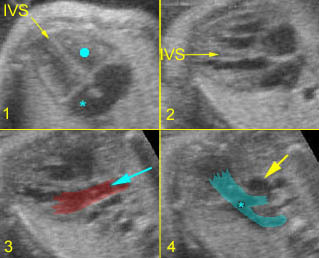
Long-axis view :
1) Four-chamber (solid circle = RV, *=LA)
2) Four-chamber view; IVS in horizontal plane
3) Ascending aorta
4) Pulmonary artery (*)
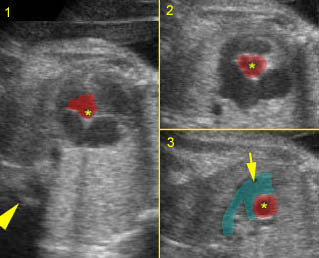
Great arteries: Sweeping
1) Aortic root from left ventricle (arrowhead = spine)
2) Short axis view: * = aorta, (arrowhead = spine)
3) Pulmonary trunk (arrow), right pulmonary artery surrounding aorta (*)
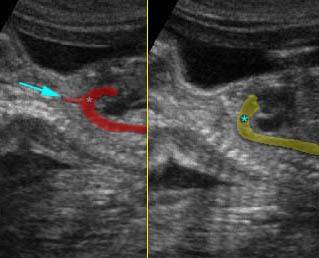
Aortic & Ductal arch :
Longitudinal view of descending aorta:
1) aortic arch (arrow = carotid artery)
2) ductal arch (*)
Full Fetal Echocardiogram
A full fetal echocardiography includes multiple views of the heart:
- Four chamber
- Long-axis left ventricle
- Short-axis great vessels
- Pulmonary artery-ductus arteriosus
- Aortic arch
- Superior and inferior vena cava
- Pulmonary veins
Additionally, color and spectral Doppler is used to identify small vessels such as the pulmonary veins and to assess valvular competence and flow patterns. Each of the views is obtained to provide specific information about the structure and/or function of the fetal heart. Inclusion of detailed fetal echocardiography as a screening examination has a substantial effect on the detection of congenital heart disease since a major proportion of prenatally detectable cases occur in a low-risk population. Attempts to perform full cardiac studies as part of routine second trimester fetal ultrasound have yielded high sensitivity rates, approximately 90% at 20-22 weeks, though fetal echocardiography can be successfully performed at 12-15 weeks of gestation permitting accurate early detection of major congenital heart defects in several cases of a high-risk population.
Tissue harmonic echocardiography seems to be the best technique to employ in obese women and in those in whom conventional ultrasound fails to provide diagnostic information. However, due its poorer resolution in women of average weight, conventional echocardiography should remain the technique of choice.
An abnormal cardiac finding during prenatal sonographic examination is a common primary indication for fetal echocardiography, accounting for 23.3% of examinations, and is more useful for identifying congenital heart disease than are other risk factors.
Increasing thickness of nuchal translucency at 11 and 14 weeks of gestation confers greater risk of congenital heart disease, even among euploid fetuses. Based on two meta-analyses, 30-56% sensitivity has been reported with a 5% false positive rate.
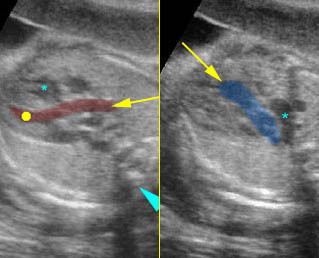
Use of Color-Flow Mapping and Pulsed Doppler
Routine use of color Doppler during every fetal cardiac examination remains controversial. Many examiners still believe that color should be reserved for cases of suspected congenital heart defect (CHD). Color-flow mapping is an important adjunct to cross-sectional scanning and can considerably speed up the cardiac evaluation. The correct direction of flow throughout the cardiac chambers and arch vessels can be demonstrated. It can be used to exclude regurgitation at any valve. At the usual Nyquist limits, unaliased color flow throughout the heart indicates that the flow is at normal velocities. If color shows aliasing at any point in the heart, pulsed Doppler should be used to obtain an accurate velocity. The peak velocity at the atrioventricular valves is 30-60 cm/sec and is fairly constant throughout gestation. The peak velocity of flow at the arterial valves is approximately 25 cm/sec at 12 weeks, increasing to 60-100 cm/sec by term. Turning on color flow when the ultrasound beam is perpendicular to the ventricular septum helps to exclude a significant ventricular septal defect. Color-flow mapping is essential to confirm a normal pulmonary venous connection. Routine use of pulsed Doppler is not necessary unless the color-flow map dictates it, but the fetal echocardiographer should be familiar with the characteristics of normal flow profiles at each point within the heart. The ultrasound beam must be positioned in-line with the flow under observation when using pulsed or color-flow mapping. This may require some technical skill. Color Doppler examination should include three cross-sectional planes: the four-chamber (4CV), five-chamber (5CV) and three-vessel (3VV) views.
Use of M-Mode Echocardiography
This modality is seldom used in fetal assessment and is not necessary during normal heart scanning. It can be used to assess ventricular function in the rare cases in which function is abnormal and it is useful in the evaluation of arrhythmias.
Three/Four-Dimensional Ultrasound
Three-dimensional imaging of fetal heart disease is feasible for a wide range of lesions, and may provide additional information of clinical value in some cases when compared with 2D imaging.

