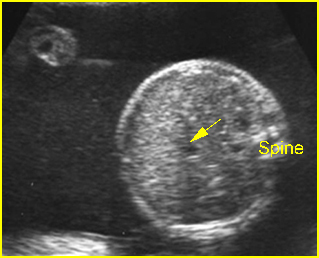
Echogenic Bowel
An increased echogenicity of bowels is associated with an increased prevalence of a variety of unfavorable outcomes including cystic fibrosis, chromosomal abnormalities such as trisomy 21, 18, 13 and triploidy, cytomegalovirus infection, intestinal obstruction, and severe fetal growth restriction. Finally, this is also commonly normal variant.
The incidence of intrauterine fetal demise in fetuses with unexplained echogenic bowel is also increased. However, there is no evidence of any serious long-term bowel pathology associated with isolated fetal echogenic bowel.
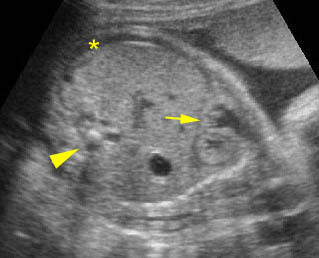
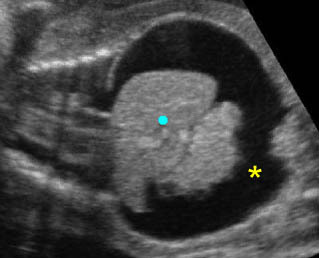
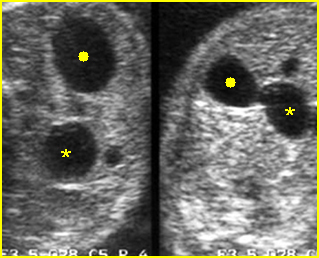
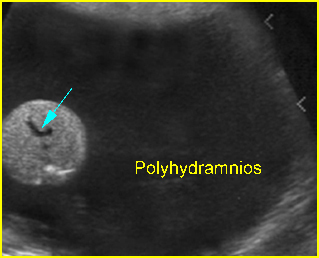
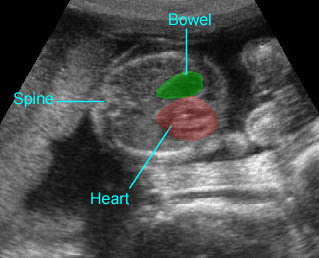
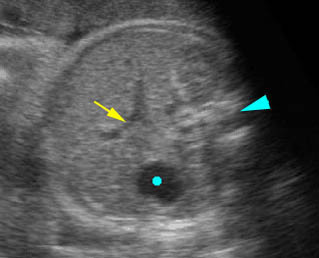
Sonographic findings:
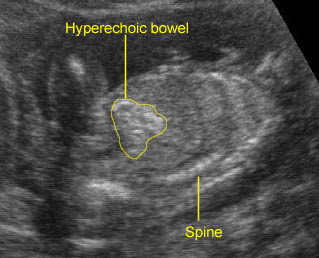
- The bowels display high echogenicity, typically occurring in the third trimester but in some cases in the second trimester.
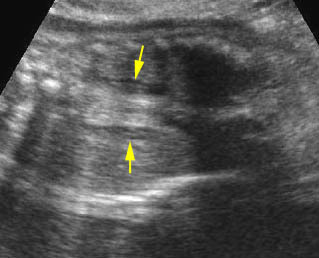
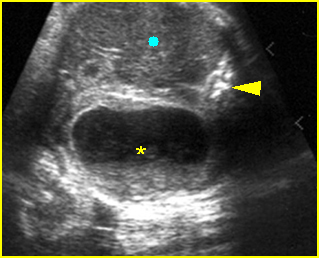
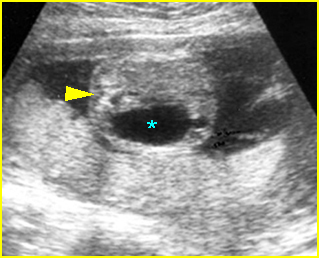
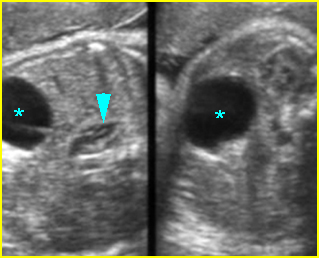
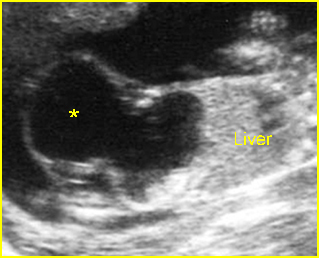
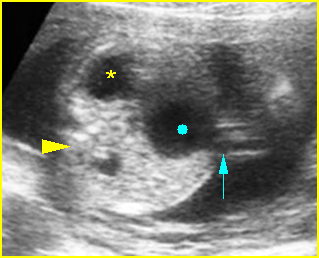
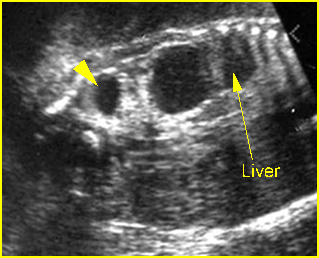
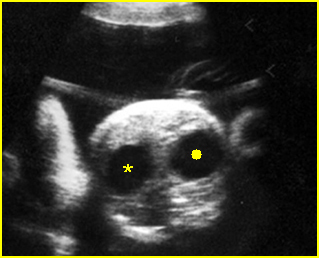
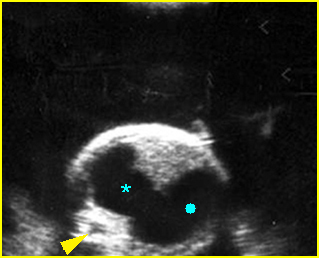
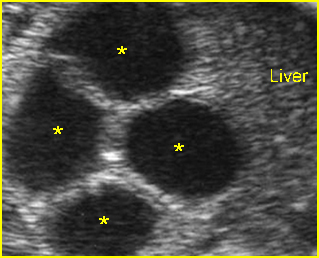
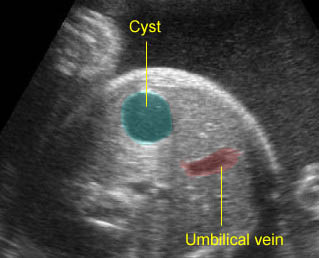
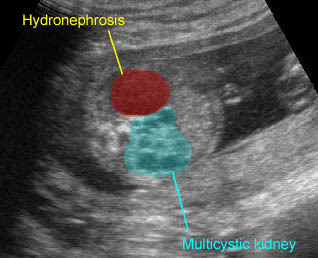
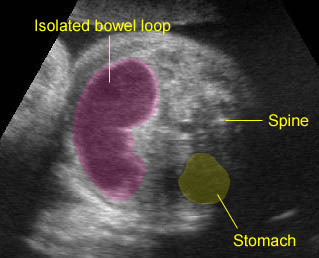
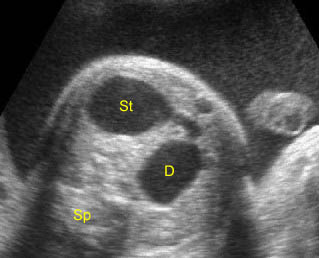
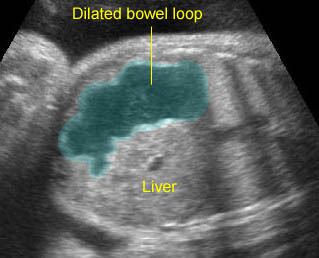
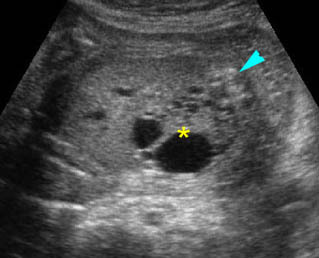
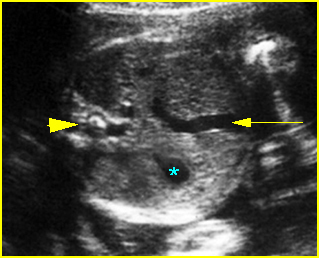
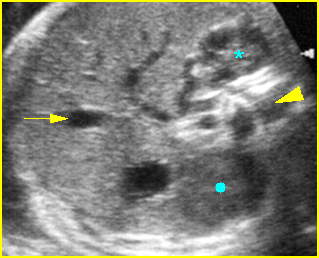
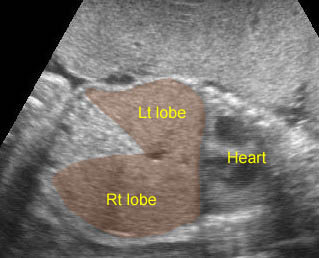
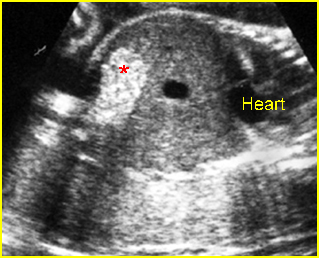
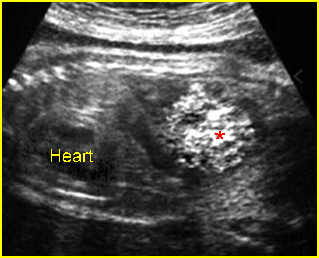
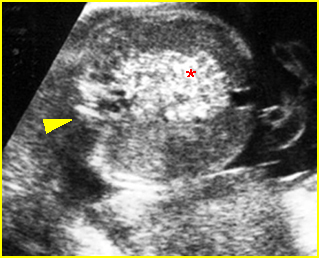
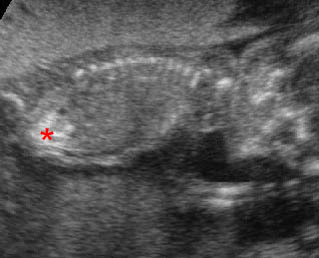
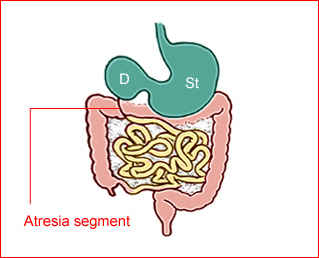
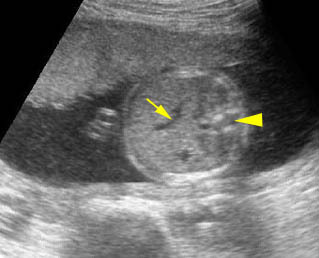
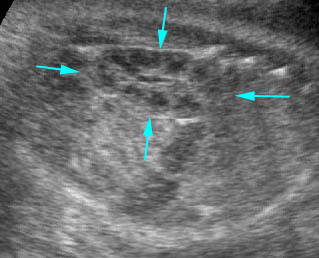
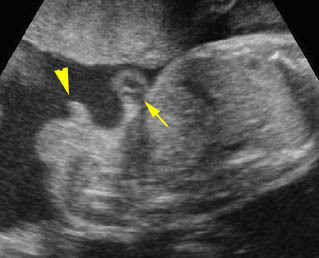
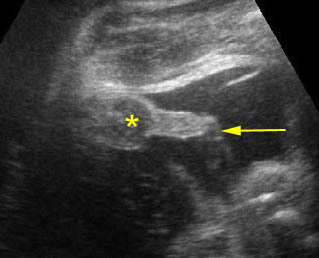
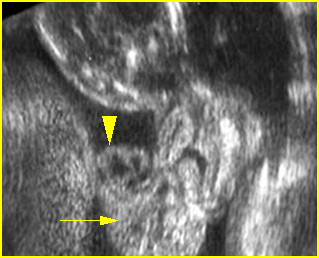
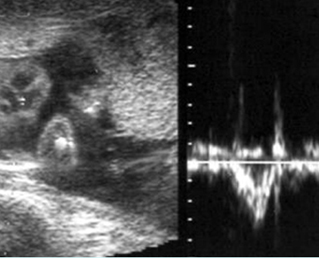
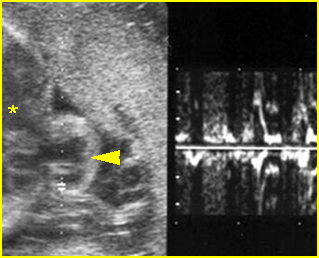
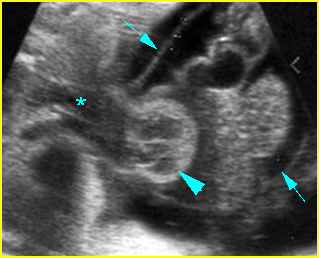
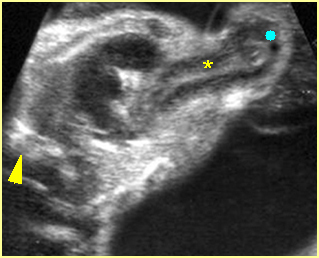
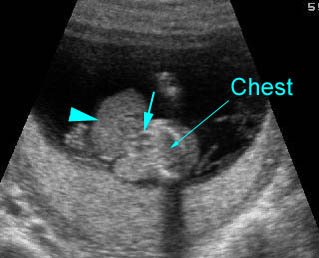
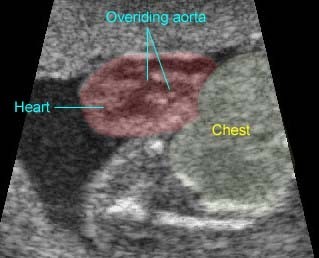
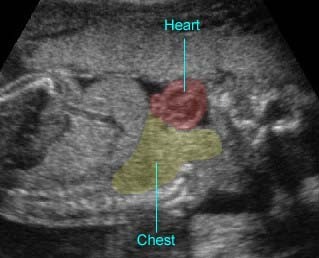
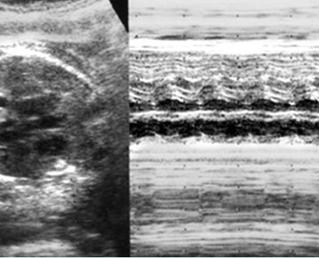
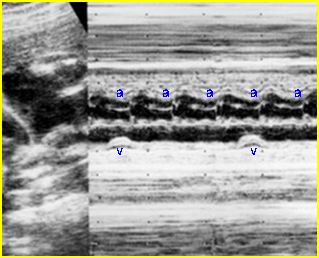
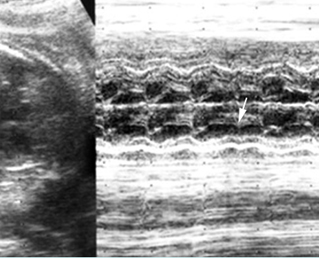
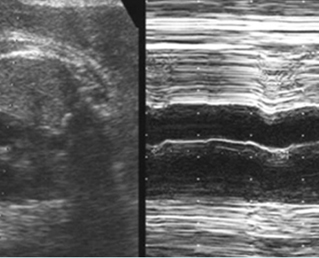
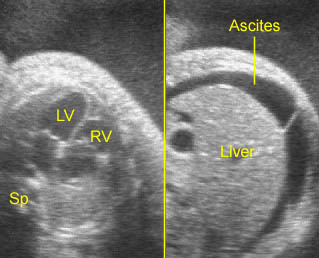
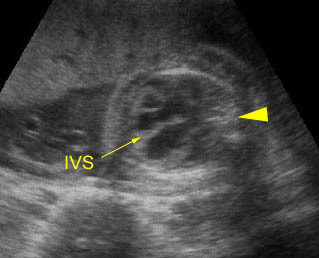
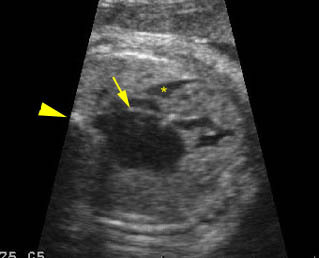
Fig 1, Fig 2, Fig 3
- Echogenic bowels should be diagnosed only when a brightness equivalent to that of the surrounding pelvic bones is achieved.
- Bowel echodensity correlates better with liver density than with bone density. Thus, comparison of bowel to liver echogenicity may be a more effective clinical tool in the evaluation of fetal intra-abdominal echodensities.
- Differential diagnosis of echogenic bowel including:
- normal variant (0.5% of normal fetuses)
- high gain settings
- bloody amniotic fluid
- meconium ileus (cystic fibrosis)
- Down’s syndrome.
Note: The use of special image processing techniques, particularly harmonic and compound-imaging techniques, can artificially enhance the apparent level of echogenicity of the bowel. Additionally, the echogenicity of normal bowel increases with transducer frequency, especially when the 8 MHz transducer is used, although this effect is uniform whereas true hyperechoic bowel tends to be focal.