4 days prior to admission, she had high-grade fever with mild degree of productive cough and runny
nose. The physical examination showed mildly injected pharynx with red enlarged tonsils. She was
diagnosed acute pharyngitis and received oral azithromycin but she still had high fever. Then, she was
admitted to provincial hospital and recevied ceftriaxone, azithromycin and ibuprofen and all infectious
tests were negative. But the fever persisted. So she was referred to Chiang Mai University hospital.
Physical examination, at 1st time of this admission
General appearance: A Thai girl with normal consciousness, febrile
Vital signs: Temperature 36.4 °C, PR 112/min, RR 32/min, BP 96/60 mmHg, Weight 15 kg
HEENT: no pale conjunctivae, no icteric sclerae, no injected conjunctivae, no injected pharynx, no
malar or discoid rash, palpable left cervical lymph node 0.5 cm in diameter, movable, no tenderness.
Chest and lungs: clear, no retraction, equal breath sound
Heart: regular rhythm, normal S1 and S2, no murmur
Abdomen: soft, no tenderness, liver was palpable 1 cm below right costal margin (RCM), sharp edge,
not tender, no palpable spleen
Extremities: no edema, no deformity, Skin: scattered erythematous papules and macules around
neck and trunk.
CBC: Hb 10.3 g/dl, Hct 31.4%, WBC 17,700/mm3, N 84.9%, L 10.3%, Ba 0.2% E 3.2%, Mo 1.4%,
platelets 244,000/mm3
ESR 80 mm/hr, CRP 297 mg/dL, UA within normal limit
She was diagnosed active SoJIA. The same dose of prednisolone was continued. Fever subsided
during the 1st day of admission. On post-admission day 2 (PD2), she developed high-grade fever
with clinical sepsis. She received cefotaxime, fluid resuscitation and prednisolone was changed to
hydrocortisone 5 times of cortisol production rate (CPR). She had fever and clinical sepsis again on
PD4 (Figure 1). CBCs were within normal limit and the investigation for sepsis was negative at both
times. Amikacin and cloxacillin were added, the latter for thrombophlebitis on PD9 but she still had
high fever. The physical examination later showed liver and spleen were palpable 4 fingerbreadth
below RCM and 2 fingerbreadth below left costal margin (LCM), respectively. There were generalized
erythematous macules and papules on the trunk and extremities (Figure 2).
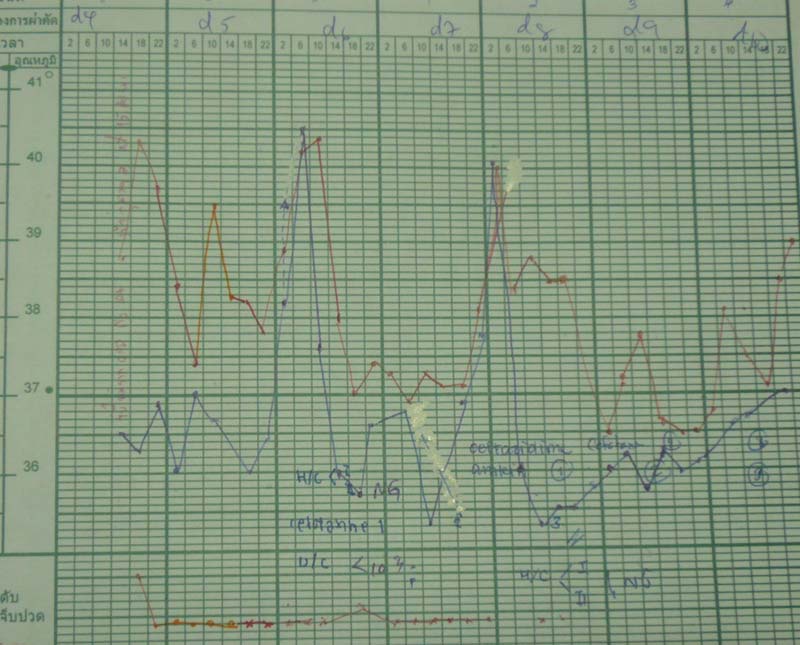
Figure 1 showed fever pattern of this patient. She had high-grade fever and clinical sepsis
on PD2 and PD4

Figure 2 showed generalized erythematous macules and papules on extremities
CBC: Hb 10.7 g/dl, Hct 32%, WBC 7,500/mm3, N 66%, band 21%, L 8%, Mo 2%, platelets
86,000/mm3
ESR 36 mm/hr
What is the diagnosis?
What is the appropriate investigation to confirm diagnosis?
Provisional diagnosis: SoJIA with macrophage activation syndrome (MAS)
Further investigation:
‐ Fibrinogen 168 mg/dL (170-405)
‐ Triglyceride 218 mg/dL (31-126)
‐ Serum ferritin 102,600 mcg/L (7-140)
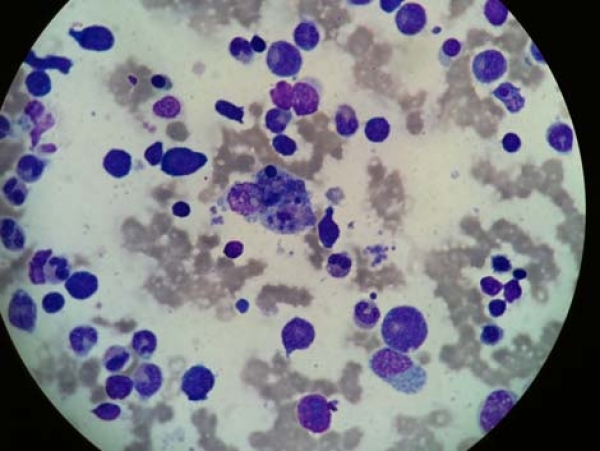
‐ Bone marrow aspiration showed normal cellularity, normal number and maturation of
megakaryocytic, erythroid and myeloid series. Blasts were less than 5%. Increased number of
histiocytes with hemophagocytic activity (Figure 3)
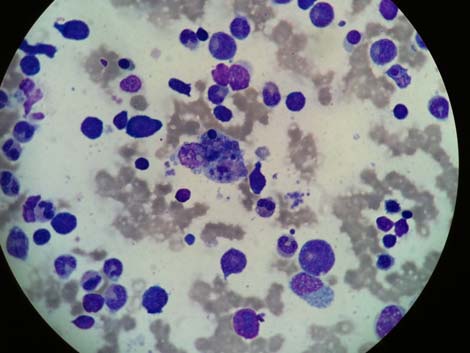
Figure 3 histiocyte with hemophagocytic activity in bone marrow (arrow)
MAS is rare but potentially fatal complication of childhood autoimmune diseases, especially SoJIA and
systemic lupus erythematosus (SLE). It is a kind of secondary hemaphagocytic histiolymphocytois (HLH).
The triggers for MAS in JIA include gold therapy, aspirin, other nonsteroidal anti-inflammatory drugs
(NSAIDs), viral and bacterial infections and autologous transplantation in patients with refractory JIA.
Pancytopenia with persistent high-spiking fever, easy bruising and bleeding, and hepatosplenomegaly
are common manifestations. So it is sometimes difficult to differentiate between two conditions, active
disease of SoJIA and MAS, due to overlap of symptoms and signs.
MAS is the result of increased number of macrophages and T cells and overproduction of cytokines.
The investigation shows hyperferritinemia (> 10,000 μg/L), pancytopenia, especially decreased
platelet and leukocyte count, elevated liver enzyme and low ESR. Patients may also have prolonged
coagulation time, low fibrinogen, increased fibrin degradation products (FDPs) and increased lactate
dehydrogenase (LDH) more than 1,000 IU/L. Presence of hemophagocytic histiocytes in bone marrow
and lymph nodes is the pathognomonic feature of this condition.
Corticosteroids are the main drug of therapy for MAS. Cyclosporine A should be added in high-risk
patients who have CNS involvement, severe bleeding diathesis, severe renal involvement, multiorgan
failure or failure response to initial therapy with corticosteroids. Etoposide and Intravenous
immunoglobulin (IVIG) may be additional options for treatment. The mortality rate of patients with
MAS was high as 8-22%.
Bibliography:
1. Arceci RJ. Bone marrow failure. In: Lanzkowsky P, ed. Manual of pediatric hematology and
oncology. 5thed. London: Elsevier,2010: p567-98.
2. Kelly A, Ramanan AV. Recognition and management of macrophage activation syndrome in
juvenile arthritis
Curr Opin Rheumatol 2007:19:477–81.
3. Davì S, Consolaro A, Guseinova D, et al. An international consensus survey of diagnostic
criteria for macrophage activation syndrome in systemic juvenile idiopathic arthritis J
Rheumatol 2011;38;764-8.
4. Ravelli A, Magni-Manzoni S, Foti T, et al. Macrophage activation syndrome in juvenile
idiopathic arthritis: towards the development of diagnostic guidelines. Arthritis Rheum
2001;44:s166.