Thanatophoric Dysplasia (TD)
Thanatophoric Dysplasia (TD)
TD is the most common lethal skeletal dysplasia in fetuses and neonates. It is caused by generalized disruption of the growth plate resulting from new autosomal dominant mutations in FGFR3. It is characterized by extreme rhizomelia, a normal trunk length with a narrow thorax, and a large head with a prominent forehead. Two subtypes have been identified:
– Type 1: severe rhizomelia, typical bowed “telephone receiver” femurs, narrow thorax, a relatively large head and absent cloverleaf skull.
– Type 2: severe cloverleaf skull and short and straight long bones.
Prenatal diagnosis with DNA analysis is currently possible.
Incidence: 1 in 4000-15,000 births, relatively increased with paternal age.
Sonographic findings:
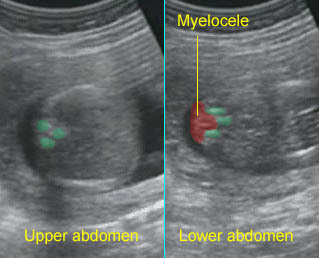
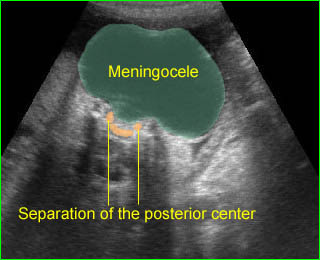
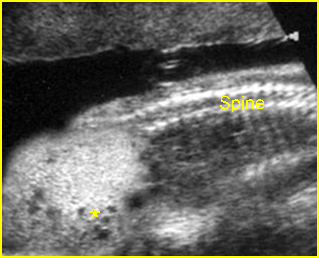
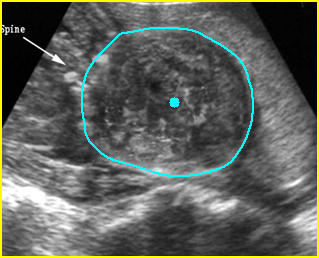
Fig 1, Fig 2, Fig 3, Fig 4, Fig 5, Fig 6
- Normal bone echodensity.
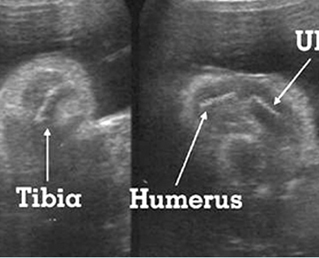
- Severe micromelia with typical telephone receiver femurs (type I).
- Long bones may grow slowly and steadily at first and stop in late pregnancy.
- Short and straight long bones (type II).
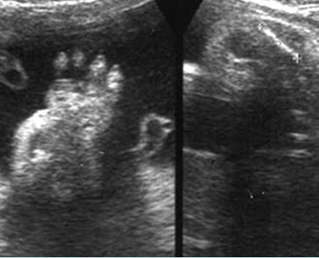
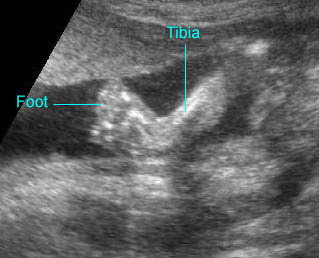
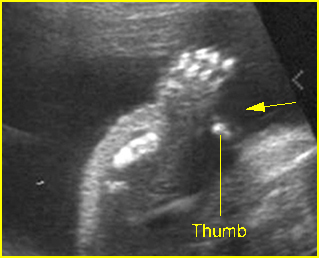
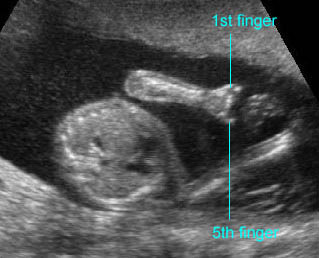
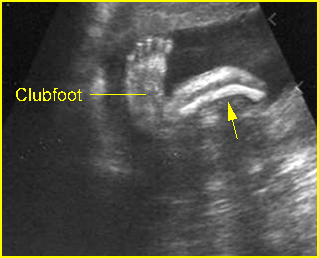
- Short and broad tubular bones in hands and feet.
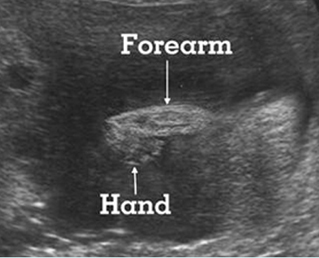
- Relatively large calvarium with a prominent forehead.
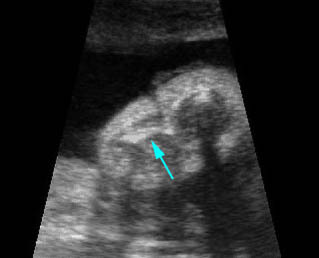
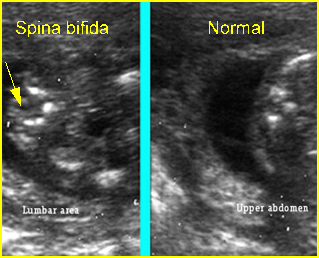
- Cloverleaf skull in about 14% of cases (all cases of type II).
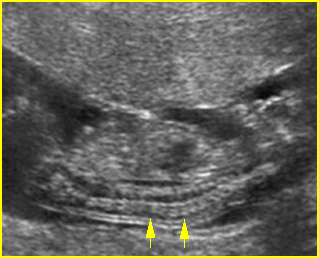
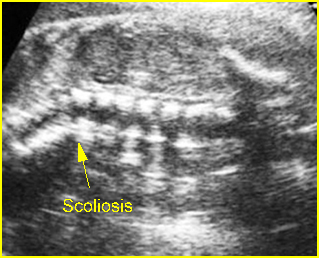
- Platyspondylosis may be documented in some cases.
- Polyhydramnios is nearly always present, especially in the third trimester.
- Ventriculomegaly in some cases.
- Increased NT in the late first trimester in some cases.
- The main differential diagnoses include all short-limbed dwarfism with normal echodensity such as short rib polydactyly syndrome, homozygous achondroplasia, and asphyxiating thoracic dysplasia (slight shortening of long bones and normal vertebrae).
- 3D ultrasound is helpful in providing more details such as the relative proportion of the appendicular skeletal elements and the hands and feet.
- Pitfalls: A normal sonographic appearance in the late first trimester can not exclude the possibility of TD.
- Usually diagnosed after the first trimester.
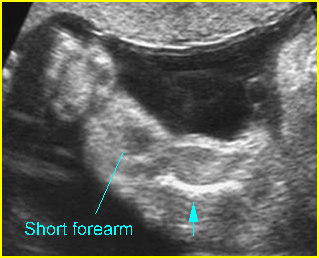
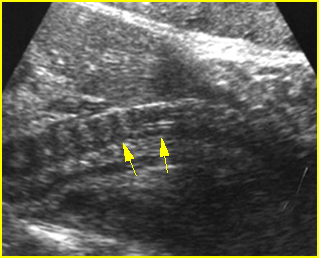
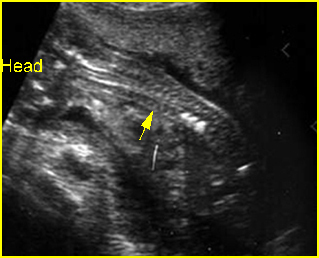
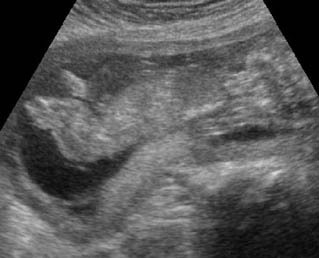
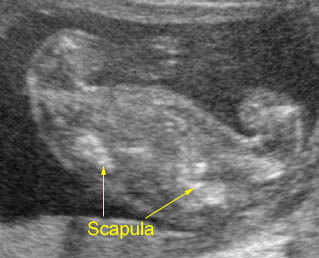
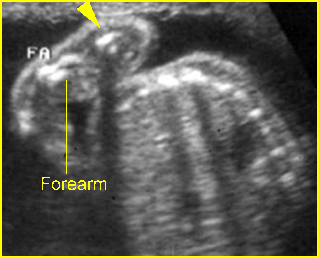
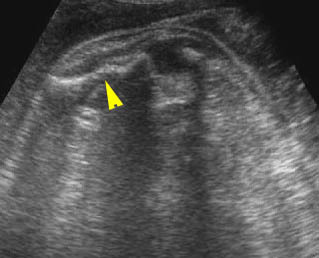
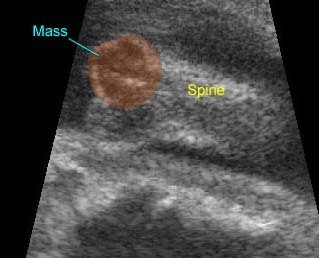
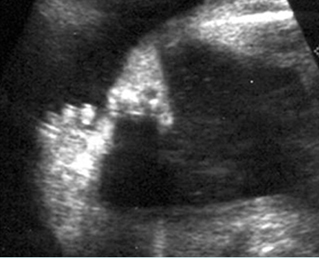
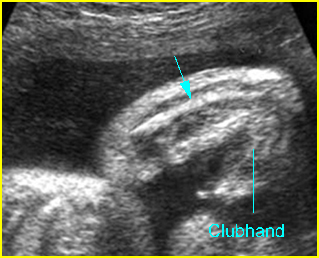
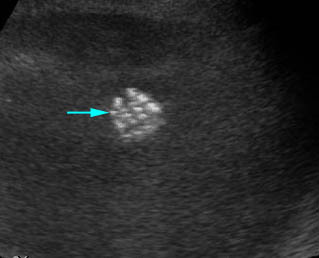
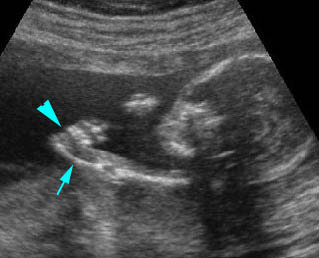
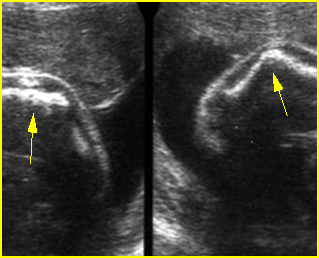
Fig 1: Micromelia in Thanatophoric dysplasia Severe shortenings of humerus (arrow) but normal ossification
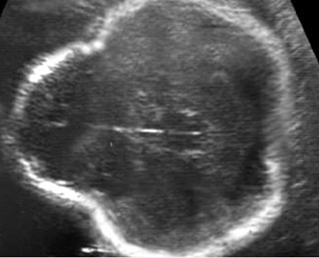
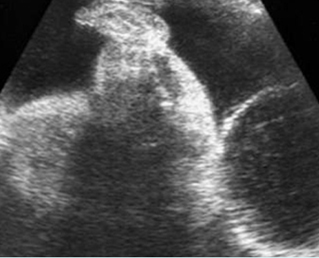
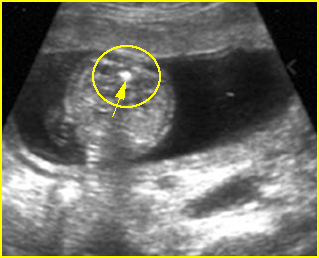
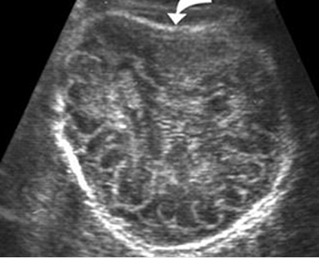
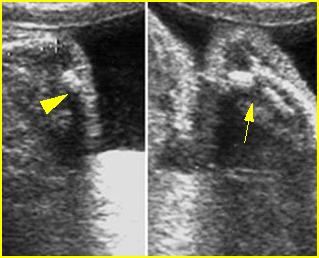
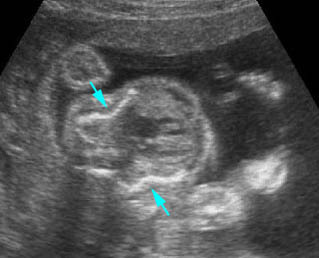
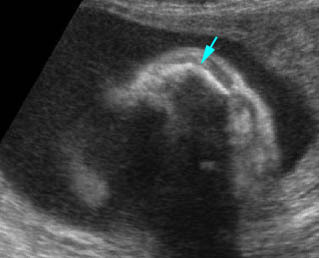
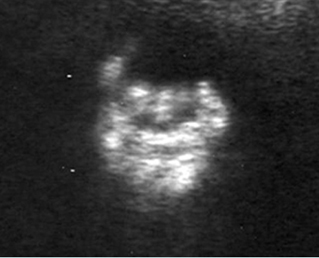
Fig 2: Thanatophoric dysplasia Cross-sectional scan of the skull: Cloverleaf skull; prominent parietal bone
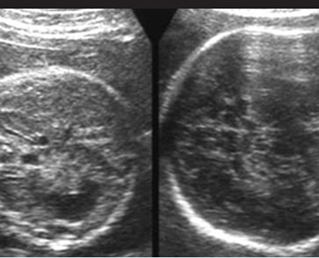
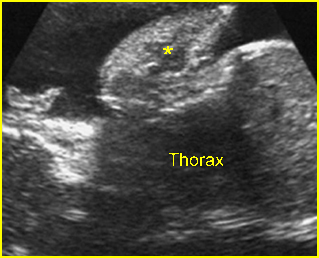
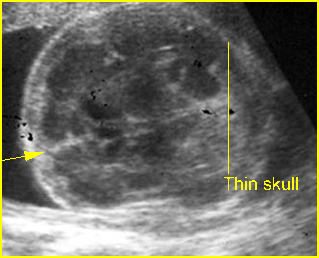
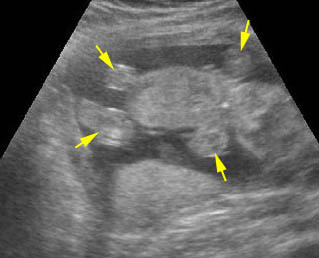
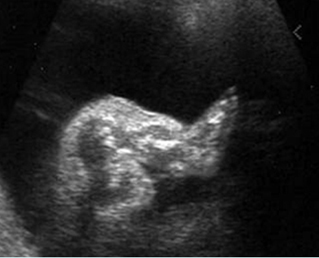
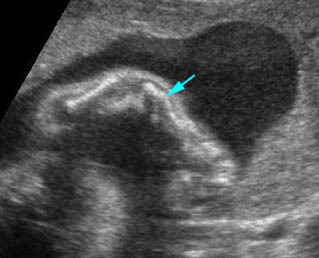
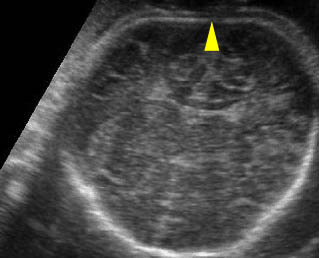
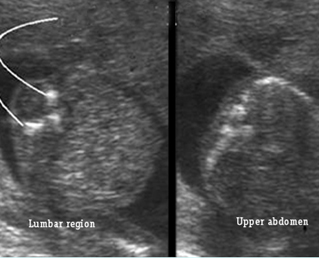
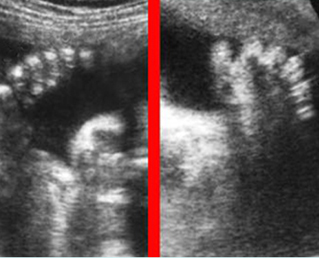
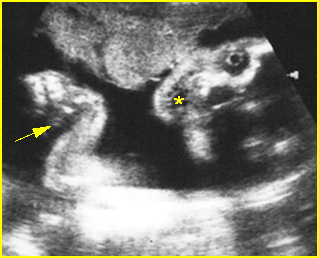
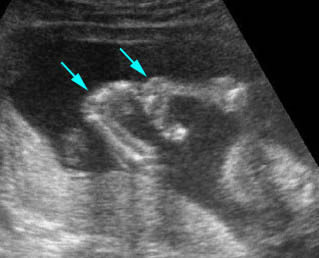
Fig 3: Large head Cross-sectional scan of the abdomen and skull: disproportion in size of the trunk and head of the fetus with Thanatophoric dysplasia
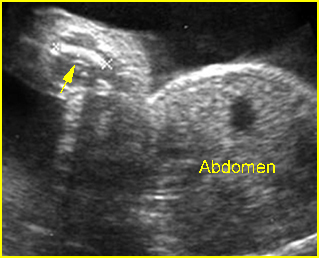
Fig 4: Micromelia in Thanatophoric dysplasia Severe shortenings of humerus (arrow) but normal ossification
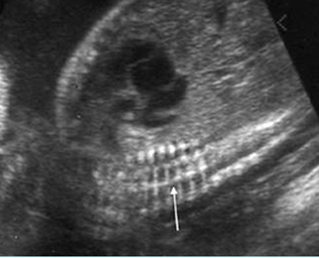
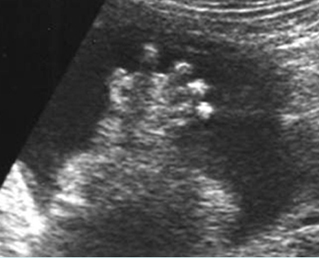
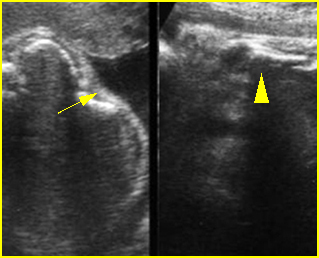
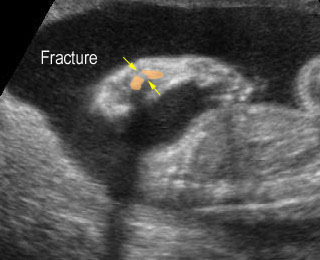
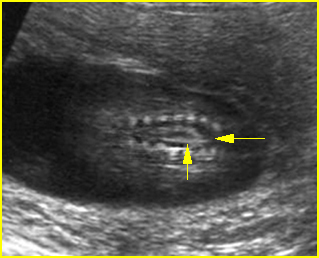
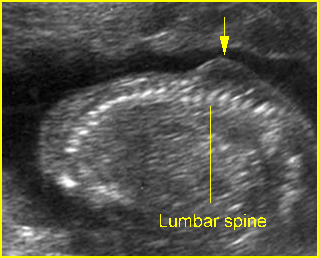
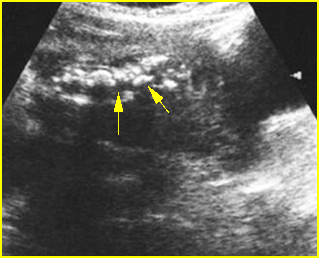
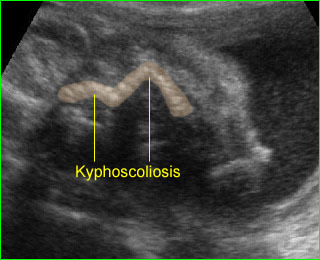
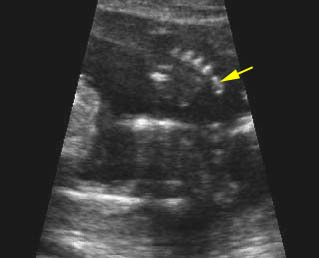
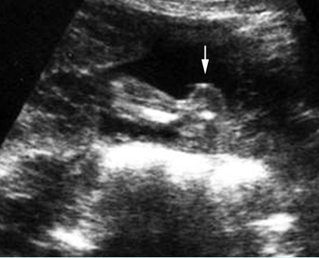
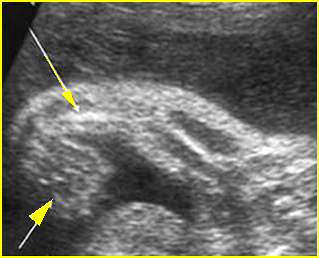
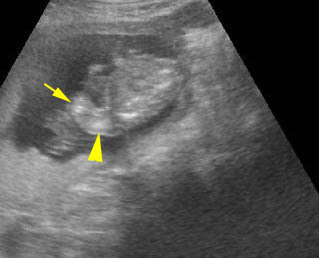
Fig 5: Platyspondylosis Oblique sagittal scan of the spine: relatively flattened vertebra (arrow) in case of Thanatophoric dysplasia
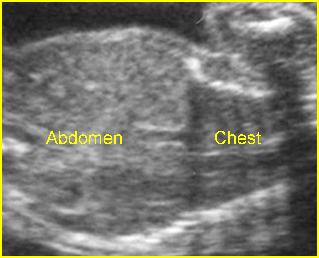
Fig 6: Small thorax in Thanatophoric dysplasia Coronal scan of fetal trunk: disproportionately small thorax, compared to the abdomen
Video clips of thanatophoric dysplasia (TD)
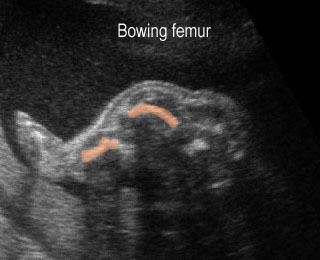
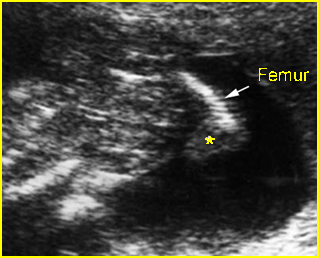
Long bone shortening : Severe long bone shortening with bowing and normal echogenicity in case of thanatophoric dysplasia
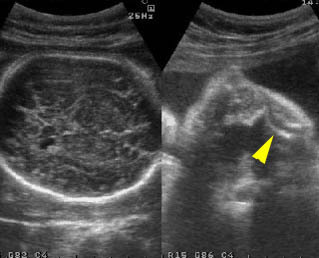
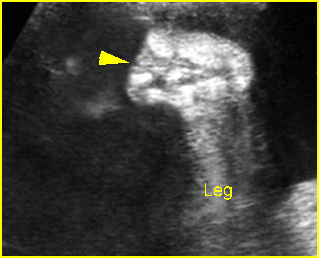
Thanatophoric dysplasia : Severe shortening of the long bone (arrowhead) compared to the skull

Thanatophoric dysplasia : Shortened femur with bowing resulting in telephone receiver appearance
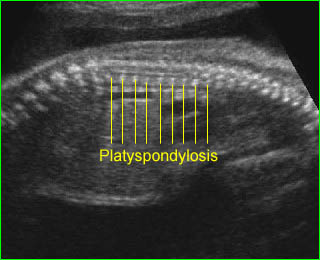
Thanatophoric dysplasia : Platyspondylosis: flattened vertebral bodies
Associations: Hydrocephalus in some cases.
Management: Termination of pregnancy can be offered.
Prognosis: Lethal; in the report of one survivor, mental and bone maturation were severely retarded.
Recurrence risk: The majority of cases are caused by new mutations, therefore, the recurrence risk is rare.